The infant of a mother with diabetes is hypoglycemic. What type of feeding should be instituted first?
D5W intravenously
Formula via nasogastric tube
Breast milk
Glucose water in a bottle
The Correct Answer is C
Choice a) D5W intravenously is incorrect because this is not the preferred method of feeding for a hypoglycemic infant. D5W stands for dextrose 5% in water, which is a solution that contains glucose and water. It can be used to treat hypoglycemia by providing a source of energy and fluid to the infant. However, it has several disadvantages, such as requiring an invasive procedure, increasing the risk of infection, causing fluid overload or electrolyte imbalance, and stimulating insulin secretion, which can lead to rebound hypoglycemia. Therefore, D5W intravenously should be reserved for severe cases of hypoglycemia that do not respond to oral or enteral feeding.
Choice b) Formula via nasogastric tube is incorrect because this is not the first-line option of feeding for a hypoglycemic infant. Formula is an artificial substitute for breast milk that contains nutrients and calories to support the infant's growth and development. It can be given via nasogastric tube, which is a tube that passes through the nose and into the stomach, when the infant cannot suck or swallow effectively. However, formula has several disadvantages, such as being less digestible, less immunogenic, and less adaptable than breast milk, as well as increasing the risk of necrotizing enterocolitis, allergy, or infection. Therefore, formula via nasogastric tube should be used only when breast milk is unavailable or contraindicated.
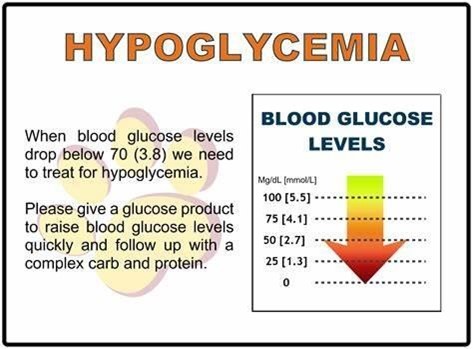
Choice c) Breast milk is correct because this is the best and most recommended type of feeding for a hypoglycemic infant. Breast milk is the natural and optimal food for infants that contains all the nutrients and antibodies they need to grow and thrive. It can be given directly from the breast or expressed and fed by bottle or cup. Breast milk has several advantages, such as being easily digestible, enhancing immune function, promoting bonding, and adjusting to the infant's needs. Breast milk also contains lactose, which is a natural sugar that can raise the blood glucose level of the infant without causing a spike in insulin secretion. Therefore, breast milk should be offered to the hypoglycemic infant as soon as possible after birth and at regular intervals thereafter.
Choice d) Glucose water in a bottle is incorrect because this is not an appropriate type of feeding for a hypoglycemic infant. Glucose water is a solution that contains glucose and water. It can be given by bottle or cup to provide a quick source of energy to the infant. However, it has several disadvantages, such as providing no other nutrients or calories, interfering with breastfeeding, causing diarrhea or dehydration, and stimulating insulin secretion, which can lead to rebound hypoglycemia. Therefore, glucose water in a bottle should be avoided or used sparingly for mild cases of hypoglycemia that do not respond to breast milk.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice a) We are protecting the infant from our bacteria is incorrect because this is not the main reason why gloves are needed when handling a newborn. While it is true that newborns have immature immune systems and are susceptible to infections, gloves are not only used to protect the infant from our bacteria but also to protect ourselves from the infant's body fluids and secretions, which may contain pathogens or blood-borne diseases.
Therefore, this response is incomplete and misleading.
Choice b) Amniotic fluid and maternal blood pose risks to us is incorrect because this is also not the primary reason why gloves are needed when handling a newborn. While it is true that amniotic fluid and maternal blood may contain harmful microorganisms or viruses that can infect us, gloves are not only used to protect ourselves from these substances but also to protect the infant from our skin flora and potential contaminants, which may cause skin irritation or infection. Therefore, this response is also incomplete and misleading.
Choice c) It is hospital policy is incorrect because this is not a sufficient or satisfactory reason why gloves are needed when handling a newborn. While it is true that wearing gloves may be a hospital policy or protocol, this response does not explain the rationale or evidence behind this policy and may imply that the nurse does not understand or agree with it. Therefore, this response is vague and unprofessional.
Choice d) It is part of standard precautions is correct because this is the best and most accurate reason why gloves are needed when handling a newborn. Standard precautions are a set of guidelines and practices that aim to prevent the transmission of infections in healthcare settings. They include wearing gloves, gowns, masks, and eye protection when there is a risk of exposure to blood or body fluids, as well as washing hands before and after patient contact, cleaning and disinfecting equipment and surfaces, and disposing of waste properly. Standard precautions apply to all patients, regardless of their diagnosis or infection status, and are based on the principle that all blood and body fluids are potentially infectious. Therefore, this response is clear and appropriate.
Correct Answer is A
Explanation
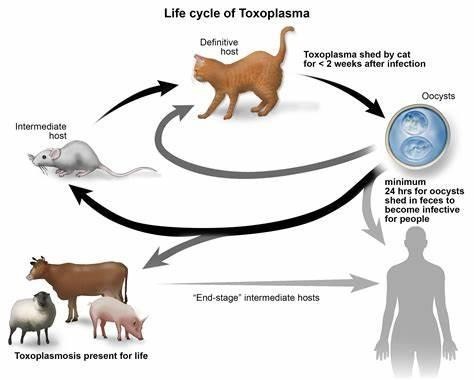
Choice a) I will be certain to empty the litter boxes regularly is incorrect because this is a risky behavior for a pregnant woman who wants to prevent toxoplasmosis. Toxoplasmosis is an infection caused by a parasite called Toxoplasma gondii, which can be found in the feces of cats and other animals. If a pregnant woman gets infected with toxoplasmosis, she can pass it to her unborn baby, which can cause serious problems such as miscarriage, stillbirth, or birth defects. Therefore, a pregnant woman should avoid contact with cat litter and let someone else handle the litter boxes, or wear gloves and wash her hands thoroughly if she has to do it herself.
Choice b) I have to wash all of my fruits and vegetables is correct because this is a good practice for a pregnant woman who wants to prevent toxoplasmosis. Toxoplasmosis can also be transmitted through contaminated soil or water, which can adhere to fruits and vegetables. Therefore, a pregnant woman should wash all of her fruits and vegetables before eating them, and peel or cook them if possible, to remove any traces of the parasite.
Choice c) I won't eat raw eggs is correct because this is another good practice for a pregnant woman who wants to prevent toxoplasmosis. Toxoplasmosis can also be acquired through eating undercooked or raw meat or eggs that contain the parasite. Therefore, a pregnant woman should avoid eating raw eggs or any foods that contain them, such as mayonnaise, mousse, or homemade ice cream, and cook all of her meat and eggs thoroughly until they are no longer pink or runny.
Choice d) I need to be cautious when cooking meat is correct because this is also an important practice for a pregnant woman who wants to prevent toxoplasmosis. Toxoplasmosis can also be spread through handling raw meat that contains the parasite. Therefore, a pregnant woman should be careful when cooking meat and use separate utensils and cutting boards for raw and cooked meat, wash her hands and surfaces after touching raw meat, and avoid tasting raw meat while cooking it.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
