The prenatal clinic nurse monitored women for preeclampsia. All four women were in the clinic at the same time. Which one should the nurse see first?
Weight gain of 0.5 kg during the past 2 weeks
Pitting pedal edema at the end of the day
Blood pressure increase to 138/86 mm Hg
Dipstick value of 3+ for protein in her urine
The Correct Answer is D
Choice A) Weight gain of 0.5 kg during the past 2 weeks: This is a normal weight gain for a pregnant woman and does not indicate preeclampsia.
Choice B) Pitting pedal edema at the end of the day: This is a common symptom of pregnancy and does not necessarily indicate preeclampsia. It can be relieved by elevating the legs and wearing compression stockings.
Choice C) Blood pressure increase to 138/86 mm Hg: This is a mild elevation of blood pressure and does not meet the criteria for preeclampsia, which is defined as a systolic blood pressure of 140 mm Hg or higher or a diastolic blood pressure of 90 mm Hg or higher on two occasions at least four hours apart.
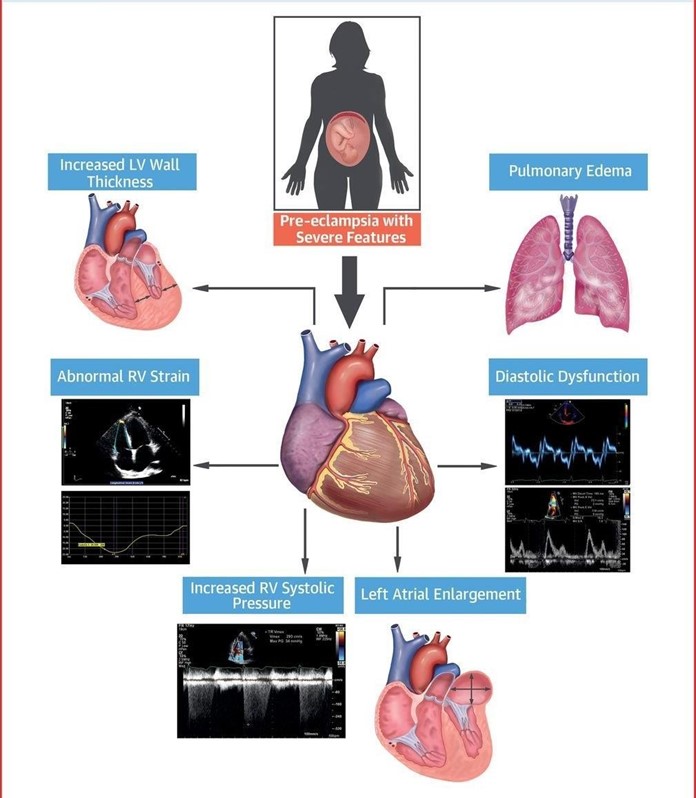
Choice D) Dipstick value of 3+ for protein in her urine: This is a sign of significant proteinuria, which is one of the main features of preeclampsia. Proteinuria is defined as a urinary protein excretion of 300 mg or more in 24 hours or a dipstick reading of 1+ or higher. A dipstick value of 3+ indicates severe proteinuria and requires immediate attention and treatment. This woman has the highest risk of developing complications from preeclampsia, such as eclampsia, HELLP syndrome, placental abruption, or fetal growth restriction . Therefore, she should be seen by the nurse first.

Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A) Antihypertensive: This is not the correct classification of magnesium sulfate. Antihypertensives are drugs that lower blood pressure, such as beta blockers, calcium channel blockers, or angiotensin-converting enzyme inhibitors. Magnesium sulfate does not have a significant effect on blood pressure, and it is not used as a primary treatment for hypertension in preeclampsia.
Choice B) Anticonvulsant: This is the correct classification of magnesium sulfate. Anticonvulsants are drugs that prevent or reduce the frequency and severity of seizures, such as phenytoin, valproic acid, or carbamazepine.
Magnesium sulfate is used as a prophylactic and therapeutic agent for eclampsia, which is a life-threatening complication of preeclampsia characterized by seizures. Magnesium sulfate acts by blocking the neuromuscular transmission and reducing the cerebral edema and vasospasm.
Choice C) Tocolytic: This is not the correct classification of magnesium sulfate. Tocolytics are drugs that inhibit uterine contractions and delay preterm labor, such as terbutaline, nifedipine, or indomethacin. Magnesium sulfate is not effective as a tocolytic agent, and it is not recommended for this purpose by the American College of Obstetricians and Gynecologists.
Choice D) Diuretic: This is not the correct classification of magnesium sulfate. Diuretics are drugs that increase urine output and reduce fluid retention, such as furosemide, hydrochlorothiazide, or spironolactone. Magnesium sulfate does not have a diuretic effect, and it can cause fluid overload and pulmonary edema if administered in excess.
Correct Answer is D
Explanation
Choice a) Insert an indwelling urinary catheter is incorrect because this is not a priority action for a client who has a large amount of painless, bright red vaginal bleeding. This type of bleeding is suggestive of placenta previa, which is a condition where the placenta covers part or all of the cervix, preventing normal delivery. Inserting an indwelling urinary catheter can cause trauma to the cervix or the placenta, which can worsen the bleeding and endanger the mother and the fetus. Therefore, this action should be avoided unless absolutely necessary.
Choice b) Prepare the abdominal and perineal areas is incorrect because this is not a priority action for a client who has a large amount of painless, bright red vaginal bleeding. This type of bleeding is suggestive of placenta previa, which is a condition where the placenta covers part or all of the cervix, preventing normal delivery. Preparing the abdominal and perineal areas can be done before performing a cesarean section, which is usually the preferred mode of delivery for placenta previa. However, this action should be done after stabilizing the client's condition and obtaining informed consent for surgery.
Choice c) Witness the signature for informed consent for surgery is incorrect because this is not a priority action for a client who has a large amount of painless, bright red vaginal bleeding. This type of bleeding is suggestive of placenta previa, which is a condition where the placenta covers part or all of the cervix, preventing normal delivery.
Witnessing the signature for informed consent for surgery can be done before performing a cesarean section, which is usually the preferred mode of delivery for placenta previa. However, this action should be done after stabilizing the client's condition and explaining the risks and benefits of surgery.
Choice d) Initiate IV access is correct because this is the priority action for a client who has a large amount of painless, bright red vaginal bleeding. This type of bleeding is suggestive of placenta previa, which is a condition where the placenta covers part or all of the cervix, preventing normal delivery. Initiating IV access can help to restore fluid volume, prevent hypovolemic shock, administer medications such as oxytocin or blood products if needed, and prepare for emergency cesarean section if indicated. Therefore, this action should be done as soon as possible to save the life of the mother and the fetus.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
