What is the result of hypothermia in the newborn?
Decreased metabolic rate
Decreased oxygen demands
Shivering to generate heat
Increased glucose demands
The Correct Answer is D
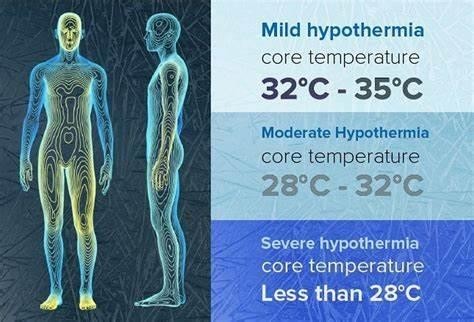
Choice A) Decreased metabolic rate is incorrect because this is not a result of hypothermia in the newborn, but rather a cause of it. Metabolic rate is the speed at which the body uses energy to perform its functions. Newborns have a high metabolic rate, which helps them to maintain a normal body temperature of 36.5°C to 37.5°C (97.7°F to 99.5°F). However, some factors can lower the metabolic rate of newborns, such as prematurity, low birth weight, infection, or hypoglycemia. A low metabolic rate can make the newborn more susceptible to heat loss and hypothermia, which is a condition that occurs when the body temperature drops below 36°C (96.8°F). Therefore, this response is inaccurate and misleading.
Choice B) Decreased oxygen demands is incorrect because this is not a result of hypothermia in the newborn, but rather a consequence of it. Oxygen demand is the amount of oxygen that the body needs to function properly.
Newborns have a high oxygen demand, which helps them to support their growth and development. However, some factors can decrease the oxygen demand of newborns, such as hypothermia, sedation, or asphyxia. A low oxygen demand can impair the oxygen delivery and utilization by the tissues and organs, leading to hypoxia, acidosis, or organ failure. Therefore, this response is irrelevant and inaccurate.
Choice C) Shivering to generate heat is incorrect because this is not a result of hypothermia in the newborn, but rather a mechanism that is absent in them. Shivering is an involuntary contraction of the muscles that produces heat and raises the body temperature. It is a common response to cold exposure in adults and older children, but not in newborns. Newborns do not have the ability to shiver, as their muscles are immature and lack glycogen stores.
Instead, they rely on other methods to generate heat, such as non-shivering thermogenesis, which involves burning brown fat in certain areas of the body. Therefore, this response is irrelevant and inaccurate.
Choice D) Increased glucose demands is correct because this is a result of hypothermia in the newborn that can cause complications. Glucose demand is the amount of glucose that the body needs to produce energy and maintain its functions. Newborns have a high glucose demand, which helps them to support their metabolic rate and thermoregulation. However, some factors can increase the glucose demand of newborns, such as hypothermia, stress, or infection. A high glucose demand can deplete the glucose stores and cause hypoglycemia, which is a low level of glucose in the blood that can lead to seizures, brain damage, or death. Therefore, this response is clear and accurate.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
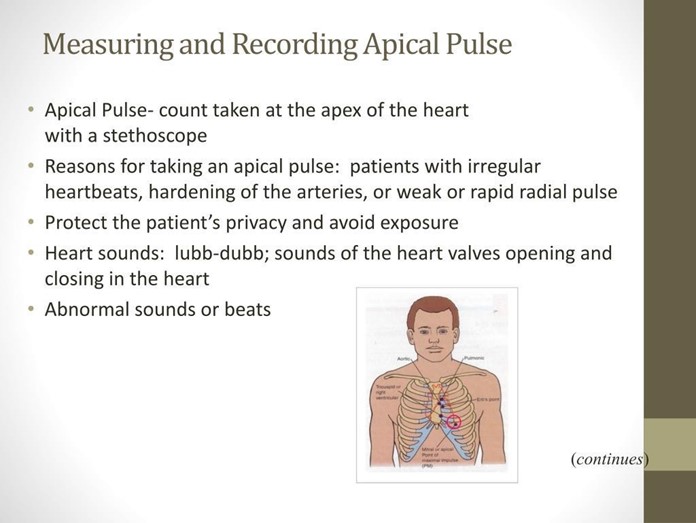
Choice a) 100 to 120 is incorrect because this is too low for a normal newborn's heart rate. The heart rate of a newborn is influenced by factors such as gestational age, activity level, temperature, and health status. A full-term, quiet, alert newborn should have a heart rate between 120 and 160 beats per minute, which reflects their high metabolic rate and oxygen demand. A heart rate below 100 beats per minute may indicate bradycardia, which can be caused by hypoxia, hypothermia, or cardiac problems.
Choice b) 120 to 160 is correct because this is the normal range for a full-term, quiet, alert newborn's heart rate. The apical pulse is the best way to measure the heart rate of a newborn, as it reflects the actual contractions of the heart. The apical pulse can be auscultated at the fourth intercostal space on the left side of the chest, just below the nipple line. The nurse should count the apical pulse for a full minute, as it may vary with the respiratory cycle.
Choice c) 80 to 100 is incorrect because this is also too low for a normal newborn's heart rate. A full-term, quiet, alert newborn should have a heart rate between 120 and 160 beats per minute, which is higher than that of an adult or an older child. A heart rate below 100 beats per minute may indicate bradycardia, which can be caused by hypoxia, hypothermia, or cardiac problems.
Choice d) 150 to 180 is incorrect because this is too high for a normal newborn's heart rate. A full-term, quiet, alert newborn should have a heart rate between 120 and 160 beats per minute, which is lower than that of a preterm or a crying newborn. A heart rate above 160 beats per minute may indicate tachycardia, which can be caused by fever, infection, anemia, or hyperthyroidism.
Correct Answer is D
Explanation
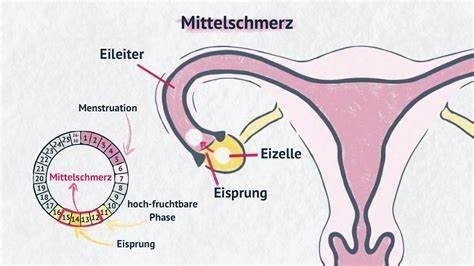
Choice a) A phase of the female menstrual cycle that involves the release of an egg (ovum) from one of the ovaries is incorrect because this is not the definition of Mittelschmerz, but rather the definition of ovulation. Ovulation is the process by which one or more eggs are released from the ovaries and travel to the fallopian tubes, where they can be fertilized by sperm. Ovulation usually occurs around the middle of the menstrual cycle, which is typically 28 days long, but can vary from person to person. Ovulation can be detected by changes in basal body temperature, cervical mucus, or hormone levels. Therefore, this response is inaccurate and misleading.
Choice B) A female reproductive organ in which ova or eggs are produced is incorrect because this is not the definition of Mittelschmerz, but rather the definition of ovary. The ovary is a paired organ that is located on either side of the uterus in the lower abdomen. The ovary contains thousands of follicles, which are sacs that contain immature eggs. Each month, one or more follicles mature and release an egg during ovulation. The ovary also produces hormones such as estrogen and progesterone, which regulate the menstrual cycle and pregnancy. Therefore, this response is irrelevant and inaccurate.
Choice C) The regular discharge of blood and mucosal tissue from the inner lining of the uterus through the vagina is incorrect because this is not the definition of Mittelschmerz, but rather the definition of menstruation. Menstruation is the process by which the endometrium, which is the tissue that lines the uterus and prepares for implantation of a fertilized egg, is shed and expelled through the vagina if pregnancy does not occur. Menstruation usually occurs once a month and lasts for about 3 to 7 days, but can vary from person to person. Menstruation can be accompanied by symptoms such as cramps, bloating, mood swings, or headaches. Therefore, this response is irrelevant and inaccurate.
Choice D) One-sided, lower belly pain associated with normal ovulation. Usually occurs about 14 days before the next menstrual period is correct because this is the definition of Mittelschmerz. Mittelschmerz is a German word that means "middle pain". It refers to a mild to moderate pain or discomfort that some women experience in their lower abdomen around the time of ovulation. The pain may last for a few minutes to a few hours and may switch sides from month to month depending on which ovary releases an egg. The pain may be caused by irritation or stretching of the ovarian or abdominal wall by the maturing follicle or by fluid or blood released during ovulation.
Mittelschmerz is not a sign of any disease or problem and does not require any treatment. However, it can be confused with other conditions that cause pelvic pain, such as appendicitis, ectopic pregnancy, or ovarian cysts. Therefore, women who have severe or persistent pain should consult their doctor for diagnosis and treatment. Therefore, this response is clear and accurate.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
