A nurse is caring for a pregnant woman at 30 weeks of gestation in preterm labor. The woman's physician orders
betamethasone 12 mg IM for two doses, with the first dose to begin at 11 am. In implementing this order, the nurse should:
Consult the physician, because the dose is too high.
Schedule the second dose for 11 am on the next day.
Prepare to administer the medication intramuscularly between contractions.
The Correct Answer is C
Choice a) Consult the physician, because the dose is too high is incorrect because this is not a necessary or appropriate action for a nurse who is following a valid order for betamethasone. Betamethasone is a corticosteroid that can be used to accelerate fetal lung maturation and reduce the risk of respiratory distress syndrome and other complications in preterm infants. The recommended dose for betamethasone is 12 mg IM every 24 hours for two doses, which is exactly what the physician ordered. Therefore, there is no reason to question or consult the physician about the dose, as it is within the normal range and based on evidence-based practice.
Choice b) Schedule the second dose for 11 am on the next day is incorrect because this is not a correct or accurate way to implement the order for betamethasone. Betamethasone should be given at least 24 hours apart, but not more than 48 hours apart, to achieve optimal fetal lung development and neonatal outcomes. Scheduling the second dose for 11 am on the next day would result in a 24-hour interval between the doses, which is acceptable, but not ideal. The best time to schedule the second dose would be between 24 and 48 hours after the first dose, such as at 11 pm on the same day or at 7 am on the next day.
Choice c) Prepare to administer the medication intramuscularly between contractions is correct because this is the best and most appropriate way to implement the order for betamethasone. Betamethasone should be given by intramuscular injection in a large muscle mass, such as the deltoid or gluteus, using a 21-gauge needle and a syringe with an air lock. The injection site should be cleaned with alcohol and aspirated before injecting. The medication should be administered between contractions, when the uterine blood flow is maximal and the fetal absorption is optimal. The nurse should also monitor the woman and the fetus for any adverse effects of betamethasone, such as maternal hyperglycemia, hypertension, infection, or edema, or fetal tachycardia, hypoglycemia, or infection.
Choice d) Explain to the woman that this medication will reduce her heart rate and help her to breathe easier is incorrect because this is not a true or relevant statement about betamethasone. Betamethasone does not have any direct effect on the maternal heart rate or respiratory function, as it is mainly intended to improve the fetal lung maturation and reduce the risk of respiratory distress syndrome and other complications in preterm infants.
Betamethasone may cause some side effects such as increased blood pressure, blood sugar, or fluid retention in the mother, which may affect her cardiovascular or respiratory status indirectly. However, these effects are usually transient and mild, and do not outweigh the benefits of betamethasone for the fetus. Therefore, this statement is misleading and inaccurate.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
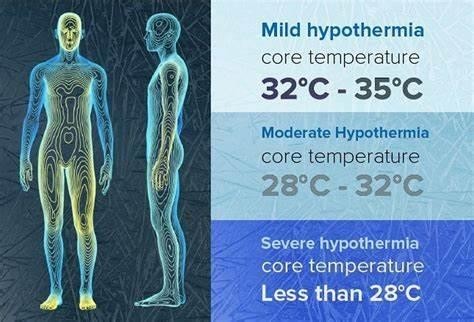
Choice A) Decreased metabolic rate is incorrect because this is not a result of hypothermia in the newborn, but rather a cause of it. Metabolic rate is the speed at which the body uses energy to perform its functions. Newborns have a high metabolic rate, which helps them to maintain a normal body temperature of 36.5°C to 37.5°C (97.7°F to 99.5°F). However, some factors can lower the metabolic rate of newborns, such as prematurity, low birth weight, infection, or hypoglycemia. A low metabolic rate can make the newborn more susceptible to heat loss and hypothermia, which is a condition that occurs when the body temperature drops below 36°C (96.8°F). Therefore, this response is inaccurate and misleading.
Choice B) Decreased oxygen demands is incorrect because this is not a result of hypothermia in the newborn, but rather a consequence of it. Oxygen demand is the amount of oxygen that the body needs to function properly.
Newborns have a high oxygen demand, which helps them to support their growth and development. However, some factors can decrease the oxygen demand of newborns, such as hypothermia, sedation, or asphyxia. A low oxygen demand can impair the oxygen delivery and utilization by the tissues and organs, leading to hypoxia, acidosis, or organ failure. Therefore, this response is irrelevant and inaccurate.
Choice C) Shivering to generate heat is incorrect because this is not a result of hypothermia in the newborn, but rather a mechanism that is absent in them. Shivering is an involuntary contraction of the muscles that produces heat and raises the body temperature. It is a common response to cold exposure in adults and older children, but not in newborns. Newborns do not have the ability to shiver, as their muscles are immature and lack glycogen stores.
Instead, they rely on other methods to generate heat, such as non-shivering thermogenesis, which involves burning brown fat in certain areas of the body. Therefore, this response is irrelevant and inaccurate.
Choice D) Increased glucose demands is correct because this is a result of hypothermia in the newborn that can cause complications. Glucose demand is the amount of glucose that the body needs to produce energy and maintain its functions. Newborns have a high glucose demand, which helps them to support their metabolic rate and thermoregulation. However, some factors can increase the glucose demand of newborns, such as hypothermia, stress, or infection. A high glucose demand can deplete the glucose stores and cause hypoglycemia, which is a low level of glucose in the blood that can lead to seizures, brain damage, or death. Therefore, this response is clear and accurate.
Correct Answer is D
Explanation
A. Dressing the infant in only a T-shirt and diaper is not recommended during phototherapy because it reduces the amount of skin exposed to the light, which is necessary for effective treatment. The infant should be minimally clothed to maximize light exposure.
B. Restricting parental and oral fluids is incorrect. Adequate hydration is crucial during phototherapy to prevent dehydration, as the treatment can increase fluid loss through the skin.
C. Keeping the infant supine at all times is not necessary. The infant should be repositioned frequently to ensure all areas of the skin are exposed to the phototherapy light, which helps in reducing bilirubin levels more effectively.
D. Keeping the infant's eyes covered under the light is essential to protect the eyes from potential damage caused by the intense phototherapy light. This is a standard practice to prevent retinal damage and other eye complications.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
