The priority nursing intervention when admitting a pregnant woman who has experienced a bleeding episode in late pregnancy is:
Monitor uterine contractions.
Assess fetal heart rate (FHR) and maternal vital signs.
Perform a venipuncture for hemoglobin and hematocrit levels.
Place clean disposable pads to collect any drainage.
The Correct Answer is B
Choice A) Monitor uterine contractions is incorrect because this is not the most urgent intervention for a pregnant woman who has experienced a bleeding episode in late pregnancy. Uterine contractions can indicate labor or placental abruption, which are possible causes of bleeding in late pregnancy. However, they are not the only or the most reliable indicators of these conditions, as some women may have painless bleeding or contractions without bleeding. Moreover, monitoring uterine contractions does not address the immediate needs of the mother and the fetus, such as oxygenation, circulation, and perfusion. Therefore, this intervention should be done after assessing and stabilizing the vital signs and FHR.
Choice B) Assess fetal heart rate (FHR) and maternal vital signs is correct because this is the most important and essential intervention for a pregnant woman who has experienced a bleeding episode in late pregnancy. Bleeding in late pregnancy can be caused by various conditions, such as placenta previa, placental abruption, uterine rupture, or vasa previa, which can compromise the blood supply and oxygen delivery to the mother and the fetus. Assessing FHR and maternal vital signs can help to determine the severity and cause of the bleeding, as well as guide further
interventions such as fluid resuscitation, oxygen therapy, blood transfusion, or emergency delivery. The normal FHR range for a fetus is 110 to 160 beats per minute, and it may vary with fetal activity or maternal position. The normal maternal vital signs are: blood pressure 120/80 mm Hg or lower, heart rate 60 to 100 beats per minute, respiratory rate 12 to 20 breaths per minute, and temperature 36.5°C to 37.5°C (97.7°F to 99.5°F). Any deviation from these ranges may indicate hypoxia, hypovolemia, shock, infection, or distress. Therefore, this intervention should be done as soon as possible for women who have bleeding in late pregnancy.
Choice c) Perform a venipuncture for hemoglobin and hematocrit levels is incorrect because this is not a priority intervention for a pregnant woman who has experienced a bleeding episode in late pregnancy. Hemoglobin and hematocrit are blood tests that measure the amount of red blood cells and their percentage in the blood volume.
They can help to evaluate the extent of blood loss and the need for blood transfusion. However, they are not
immediate or accurate indicators of bleeding in late pregnancy, as they may take time to reflect the changes in blood volume or be affected by other factors such as hydration or hemodilution. Moreover, performing a venipuncture does not address the immediate needs of the mother and the fetus, such as oxygenation, circulation, and perfusion.
Therefore, this intervention should be done after assessing and stabilizing the vital signs and FHR.
Choice d) Place clean disposable pads to collect any drainage is incorrect because this is not a priority intervention for a pregnant woman who has experienced a bleeding episode in late pregnancy. Placing clean disposable pads can help to keep the perineal area clean and dry, as well as to estimate the amount and type of bleeding. However, it does not address the immediate needs of the mother and the fetus, such as oxygenation, circulation, and perfusion. Moreover, it does not provide any information about the cause or severity of the bleeding, as it may be affected by factors such as gravity or pooling. Therefore, this intervention should be done after assessing and stabilizing the vital signs and FHR.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice a) Insert an indwelling urinary catheter is incorrect because this is not a priority action for a client who has a large amount of painless, bright red vaginal bleeding. This type of bleeding is suggestive of placenta previa, which is a condition where the placenta covers part or all of the cervix, preventing normal delivery. Inserting an indwelling urinary catheter can cause trauma to the cervix or the placenta, which can worsen the bleeding and endanger the mother and the fetus. Therefore, this action should be avoided unless absolutely necessary.
Choice b) Prepare the abdominal and perineal areas is incorrect because this is not a priority action for a client who has a large amount of painless, bright red vaginal bleeding. This type of bleeding is suggestive of placenta previa, which is a condition where the placenta covers part or all of the cervix, preventing normal delivery. Preparing the abdominal and perineal areas can be done before performing a cesarean section, which is usually the preferred mode of delivery for placenta previa. However, this action should be done after stabilizing the client's condition and obtaining informed consent for surgery.
Choice c) Witness the signature for informed consent for surgery is incorrect because this is not a priority action for a client who has a large amount of painless, bright red vaginal bleeding. This type of bleeding is suggestive of placenta previa, which is a condition where the placenta covers part or all of the cervix, preventing normal delivery.
Witnessing the signature for informed consent for surgery can be done before performing a cesarean section, which is usually the preferred mode of delivery for placenta previa. However, this action should be done after stabilizing the client's condition and explaining the risks and benefits of surgery.
Choice d) Initiate IV access is correct because this is the priority action for a client who has a large amount of painless, bright red vaginal bleeding. This type of bleeding is suggestive of placenta previa, which is a condition where the placenta covers part or all of the cervix, preventing normal delivery. Initiating IV access can help to restore fluid volume, prevent hypovolemic shock, administer medications such as oxytocin or blood products if needed, and prepare for emergency cesarean section if indicated. Therefore, this action should be done as soon as possible to save the life of the mother and the fetus.
Correct Answer is B
Explanation
Choice a) 100 to 120 is incorrect because this is too low for a normal newborn's heart rate. The heart rate of a newborn is influenced by factors such as gestational age, activity level, temperature, and health status. A full-term, quiet, alert newborn should have a heart rate between 120 and 160 beats per minute, which reflects their high metabolic rate and oxygen demand. A heart rate below 100 beats per minute may indicate bradycardia, which can be caused by hypoxia, hypothermia, or cardiac problems.
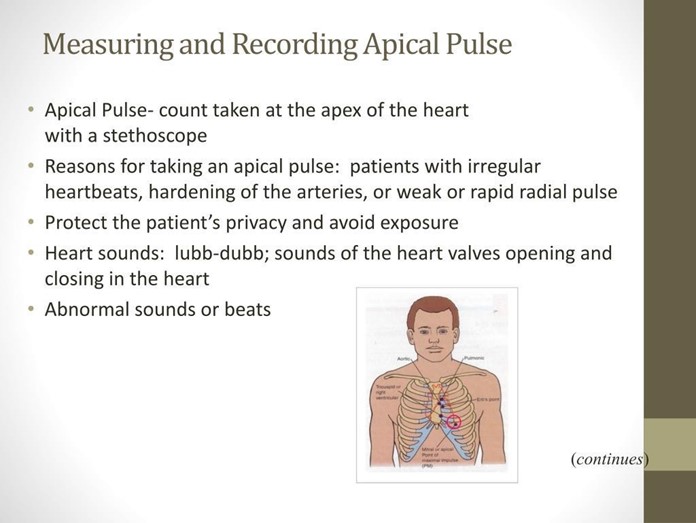
Choice b) 120 to 160 is correct because this is the normal range for a full-term, quiet, alert newborn's heart rate. The apical pulse is the best way to measure the heart rate of a newborn, as it reflects the actual contractions of the heart. The apical pulse can be auscultated at the fourth intercostal space on the left side of the chest, just below the nipple line. The nurse should count the apical pulse for a full minute, as it may vary with the respiratory cycle.
Choice c) 80 to 100 is incorrect because this is also too low for a normal newborn's heart rate. A full-term, quiet, alert newborn should have a heart rate between 120 and 160 beats per minute, which is higher than that of an adult or an older child. A heart rate below 100 beats per minute may indicate bradycardia, which can be caused by hypoxia, hypothermia, or cardiac problems.
Choice d) 150 to 180 is incorrect because this is too high for a normal newborn's heart rate. A full-term, quiet, alert newborn should have a heart rate between 120 and 160 beats per minute, which is lower than that of a preterm or a crying newborn. A heart rate above 160 beats per minute may indicate tachycardia, which can be caused by fever, infection, anemia, or hyperthyroidism.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
