A newborn has meconium aspiration at birth. The nurse notes increasing respiratory distress. What action takes priority?
Obtain an oxygen saturation.
Stimulate the baby to increase respirations.
Prepare to initiate ECMO.
Notify the provider at once.
The Correct Answer is D
Choice A) Obtain an oxygen saturation: This is not a priority action because it does not address the underlying cause of the respiratory distress, which is meconium aspiration. Meconium aspiration can cause airway obstruction, inflammation, infection, and pulmonary hypertension in the newborn. Oxygen saturation may be low, but it is not a reliable indicator of the severity of the condition.
Choice B) Stimulate the baby to increase respirations: This is not a priority action because it may worsen the respiratory distress by increasing the work of breathing and causing more meconium to be aspirated. Stimulation may also cause stress and hypoxia in the newborn.
Choice C) Prepare to initiate ECMO: This is not a priority action because it is a last resort treatment for severe cases of meconium aspiration syndrome that do not respond to conventional therapies. ECMO stands for extracorporeal membrane oxygenation, which is a form of life support that bypasses the lungs and provides oxygen to the blood.
ECMO has many risks and complications, such as bleeding, infection, and organ damage. It should only be used when other options have failed and with the consent of the parents.
Choice D) Notify the provider at once: This is the correct action because it allows for prompt assessment and intervention by the provider, who can initiate appropriate treatments for meconium aspiration syndrome. These may include suctioning of the airway, administration of antibiotics, surfactant, or inhaled nitric oxide, and mechanical ventilation . Early treatment can improve the outcomes and reduce the complications of meconium aspiration syndrome.

Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A: This is incorrect because acetylsalicylic acid (ASA), also known as aspirin, is not a cure for preeclampsia, but a preventive measure. ASA may reduce the risk of preeclampsia in some high-risk women by inhibiting platelet aggregation and improving blood flow to the placenta. However, ASA is not recommended for all pregnant women, as it may have adverse effects on the mother and the fetus, such as bleeding, premature closure of the ductus arteriosus, or fetal growth restriction.
Choice B: This is the correct answer because delivery of the fetus is the only definitive treatment for preeclampsia, as it eliminates the source of the placental factors that cause the condition. Preeclampsia is a multisystem disorder characterized by hypertension, proteinuria, and edema that occurs after 20 weeks of gestation. It is caused by abnormal placentation and endothelial dysfunction that lead to vasoconstriction, inflammation, and coagulation.
Delivery of the fetus and the placenta resolves these abnormalities and restores normal maternal physiology.
Choice C: This is incorrect because antihypertensive medications are not a cure for preeclampsia, but a symptomatic management. Antihypertensive medications may lower the blood pressure and reduce the risk of maternal complications, such as stroke, seizure, or organ damage. However, antihypertensive medications do not address the underlying cause of preeclampsia and do not improve fetal outcomes. Moreover, some antihypertensive medications are contraindicated in pregnancy due to their teratogenic effects.
Choice D: This is incorrect because magnesium sulfate is not a cure for preeclampsia, but a prophylaxis for eclampsia. Eclampsia is a severe complication of preeclampsia that involves seizures and coma. Magnesium sulfate is an anticonvulsant that prevents or treats eclamptic seizures by stabilizing neuronal membranes and reducing cerebral edema. However, magnesium sulfate does not lower blood pressure or improve renal function in preeclamptic women. It also has side effects such as nausea, flushing, headache, or respiratory depression.

Correct Answer is A
Explanation
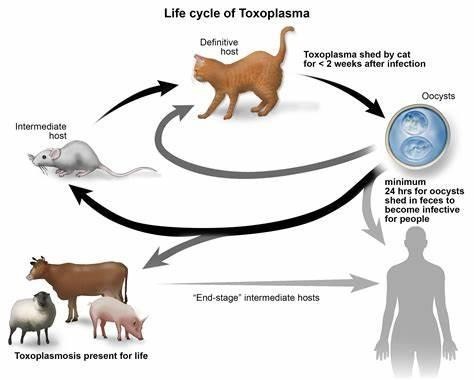
Choice a) I will be certain to empty the litter boxes regularly is incorrect because this is a risky behavior for a pregnant woman who wants to prevent toxoplasmosis. Toxoplasmosis is an infection caused by a parasite called Toxoplasma gondii, which can be found in the feces of cats and other animals. If a pregnant woman gets infected with toxoplasmosis, she can pass it to her unborn baby, which can cause serious problems such as miscarriage, stillbirth, or birth defects. Therefore, a pregnant woman should avoid contact with cat litter and let someone else handle the litter boxes, or wear gloves and wash her hands thoroughly if she has to do it herself.
Choice b) I have to wash all of my fruits and vegetables is correct because this is a good practice for a pregnant woman who wants to prevent toxoplasmosis. Toxoplasmosis can also be transmitted through contaminated soil or water, which can adhere to fruits and vegetables. Therefore, a pregnant woman should wash all of her fruits and vegetables before eating them, and peel or cook them if possible, to remove any traces of the parasite.
Choice c) I won't eat raw eggs is correct because this is another good practice for a pregnant woman who wants to prevent toxoplasmosis. Toxoplasmosis can also be acquired through eating undercooked or raw meat or eggs that contain the parasite. Therefore, a pregnant woman should avoid eating raw eggs or any foods that contain them, such as mayonnaise, mousse, or homemade ice cream, and cook all of her meat and eggs thoroughly until they are no longer pink or runny.
Choice d) I need to be cautious when cooking meat is correct because this is also an important practice for a pregnant woman who wants to prevent toxoplasmosis. Toxoplasmosis can also be spread through handling raw meat that contains the parasite. Therefore, a pregnant woman should be careful when cooking meat and use separate utensils and cutting boards for raw and cooked meat, wash her hands and surfaces after touching raw meat, and avoid tasting raw meat while cooking it.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
