Adllent, 1 day postpartum, is being monitored after a postpartum hemorrhage. Which of the following should the nurse report to the obstetrician?
Urine output of 200 mL for the past 8 hours.
Weight decrease of 2 pounds since delivery.
Pulse rate of 65 beats per minute.
Drop in hematocrit of 6% since admission.
The Correct Answer is D
Choice a) Urine output of 200 mL for the past 8 hours is incorrect because this is a normal finding for a postpartum woman. The average urine output for a healthy adult is about 800 to 2000 mL per day, which means about 100 to 250 mL per hour. Therefore, a urine output of 200 mL for the past 8 hours is within the normal range and does not indicate any complications.
Choice b) Weight decrease of 2 pounds since delivery is incorrect because this is also a normal finding for a postpartum woman. The weight loss is due to the expulsion of the placenta, amniotic fluid, and blood during delivery. A postpartum woman can expect to lose about 10 to 12 pounds immediately after giving birth, and another 5 pounds in the following weeks due to fluid loss. Therefore, a weight decrease of 2 pounds since delivery is not a cause for concern and does not need to be reported to the obstetrician.
Choice c) Pulse rate of 65 beats per minute is incorrect because this is also a normal finding for a postpartum woman. The normal resting pulse rate for an adult ranges from 60 to 100 beats per minute, and it may decrease slightly after delivery due to blood loss and reduced cardiac output. Therefore, a pulse rate of 65 beats per minute is not indicative of any problems and does not require any intervention.
Choice d) Drop in hematocrit of 6% since admission is correct because this is an abnormal finding for a postpartum woman and suggests that she has developed anemia due to excessive blood loss. Hematocrit is the percentage of red blood cells in the blood, and it reflects the oxygen-carrying capacity of the blood. The normal hematocrit range for an adult female is 37% to 47%, and it may decrease slightly after delivery due to hemodilution. However, a drop in hematocrit of more than 10% from the baseline or below 30% indicates severe anemia and requires immediate treatment. Therefore, a drop in hematocrit of 6% since admission is a significant change that should be reported to the obstetrician as soon as possible.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
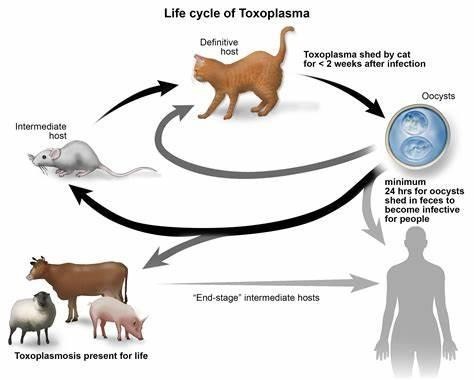
Choice a) I will be certain to empty the litter boxes regularly is incorrect because this is a risky behavior for a pregnant woman who wants to prevent toxoplasmosis. Toxoplasmosis is an infection caused by a parasite called Toxoplasma gondii, which can be found in the feces of cats and other animals. If a pregnant woman gets infected with toxoplasmosis, she can pass it to her unborn baby, which can cause serious problems such as miscarriage, stillbirth, or birth defects. Therefore, a pregnant woman should avoid contact with cat litter and let someone else handle the litter boxes, or wear gloves and wash her hands thoroughly if she has to do it herself.
Choice b) I have to wash all of my fruits and vegetables is correct because this is a good practice for a pregnant woman who wants to prevent toxoplasmosis. Toxoplasmosis can also be transmitted through contaminated soil or water, which can adhere to fruits and vegetables. Therefore, a pregnant woman should wash all of her fruits and vegetables before eating them, and peel or cook them if possible, to remove any traces of the parasite.
Choice c) I won't eat raw eggs is correct because this is another good practice for a pregnant woman who wants to prevent toxoplasmosis. Toxoplasmosis can also be acquired through eating undercooked or raw meat or eggs that contain the parasite. Therefore, a pregnant woman should avoid eating raw eggs or any foods that contain them, such as mayonnaise, mousse, or homemade ice cream, and cook all of her meat and eggs thoroughly until they are no longer pink or runny.
Choice d) I need to be cautious when cooking meat is correct because this is also an important practice for a pregnant woman who wants to prevent toxoplasmosis. Toxoplasmosis can also be spread through handling raw meat that contains the parasite. Therefore, a pregnant woman should be careful when cooking meat and use separate utensils and cutting boards for raw and cooked meat, wash her hands and surfaces after touching raw meat, and avoid tasting raw meat while cooking it.
Correct Answer is B
Explanation
Choice A: This is incorrect because Standard Precautions are a set of guidelines that apply to all patients, regardless of their infection status. They include using personal protective equipment, handling sharps and waste properly, and cleaning and disinfecting equipment and surfaces. However, they are not enough to prevent neonatal infection, as some pathogens can still be transmitted by contact or droplet.
Choice B: This is the correct answer because good hand hygiene is the most effective way to prevent the transmission of microorganisms that can cause neonatal infection. The nurse should wash their hands with soap and water or use an alcohol-based hand rub before and after touching the infant, the infant's environment, or any items that come in contact with the infant. The nurse should also educate the parents and visitors on the importance of hand hygiene and how to perform it correctly.
Choice C: This is incorrect because a separate gown technique involves wearing a clean gown for each infant and discarding it after use. This can help prevent cross-contamination between infants, but it does not eliminate the need for hand hygiene. The nurse should still wash their hands before and after wearing a gown, as well as before and after touching the infant or any items that come in contact with the infant.
Choice D: This is incorrect because isolation of infected infants involves placing them in a separate room or area with restricted access and using additional precautions based on the mode of transmission of the infection. This can help prevent the spread of infection to other infants, staff, or visitors, but it does not eliminate the need for hand hygiene. The nurse should still wash their hands before and after entering and leaving the isolation area, as well as before and after touching the infant or any items that come in contact with the infant.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
