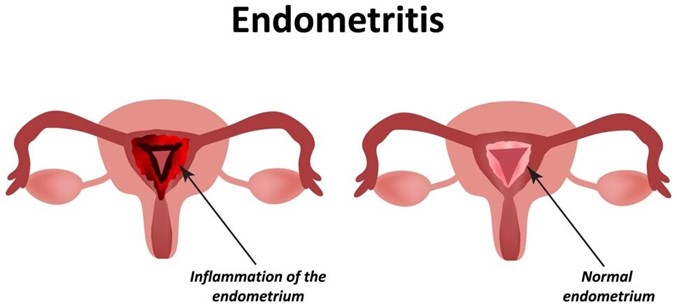
A nurse is assessing a client who is 6 hours postpartum and has endometritis. Which of the following findings should the nurse expect?
Temperature 37.4°C (99.3°F)
Scant lochia
Uterine tenderness
WBC count 9,000/mm³
The Correct Answer is C
Endometritis is an infection of the endometrium, the lining of the uterus, typically occurring after childbirth. When assessing a client with endometritis, the nurse should expect to find uterine tenderness as a common clinical finding. This finding is consistent with endometritis, which is characterized by inflammation and infection of the endometrium. Additional signs and symptoms may include an elevated temperature, increased lochia, foul-smelling lochia, and an elevated WBC count. Prompt identification and treatment of endometritis are important to prevent further complications.
Option a) A temperature of 37.4°C (99.3°F) is within the normal range and does not necessarily indicate endometritis. However, an elevated temperature above 38°C (100.4°F) or a persistent fever may be indicative of an infection and should be further evaluated.
Option b) Scant lochia (minimal vaginal bleeding) is not a characteristic finding of endometritis. In endometritis, lochia is often increased in amount and may have an unpleasant odor.
Option d) A white blood cell (WBC) count of 9,000/mm³ is within the normal range. However, in cases of endometritis, there is usually an elevation in the WBC count as a response to the infection. An elevated or increasing WBC count may be observed.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
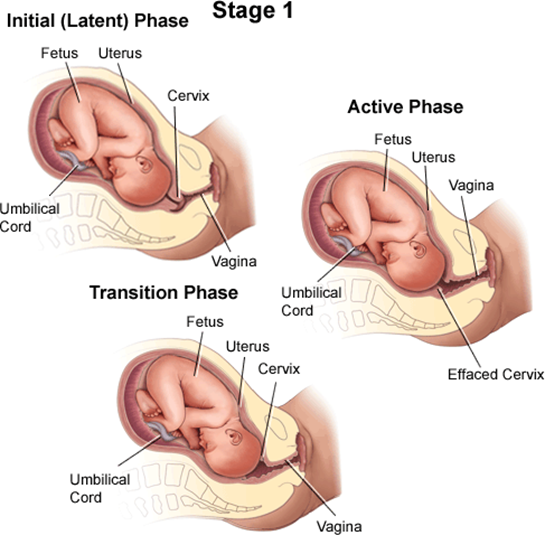
A client who is in labor and reports an urge to have a bowel movement during contractions may be experiencing the transition phase of labor, which is the last and most intense part of the first stage of labor¹². The transition phase occurs when the cervix dilates from 8 to 10 cm and the baby descends into the birth canal¹². The pressure of the baby's head on the rectum can cause a sensation of needing to defecate¹². The transition phase can last from 15 minutes to an hour or more, and it can be accompanied by other signs, such as strong, regular, and painful contractions lasting 60 to 90 seconds; increased bloody show; nausea and vomiting; shaking and shivering; and emotional changes such as irritability, anxiety, or excitement¹²³.
The nurse should reassess the client who reports an urge to have a bowel movement during contractions because this may indicate that the client is close to delivering the baby and needs to be prepared for the second stage of labor, which involves pushing and giving birth¹². The nurse should check the client's cervical dilation, fetal heart rate, and maternal vital signs, and notify the provider if the client is fully dilated or shows signs of fetal or maternal distress¹². The nurse should also support the client's coping strategies, such as breathing techniques, relaxation methods, or pain relief options, and encourage the client not to push until instructed by the provider¹².
b) A sense of excitement and warm, flushed skin are not signs that require reassessment by the nurse. These are normal emotional and physiological responses to labor that reflect increased adrenaline levels and blood flow¹⁴. They do not indicate any complications or imminent delivery.
c) Progressive sacral discomfort during contractions is not a sign that requires reassessment by the nurse. This is a common symptom of labor that results from the pressure of the baby's head on the sacrum and nerves in the lower back¹⁴. It does not indicate any problems or imminent delivery.
d) Intense contractions lasting 45 to 60 seconds are not signs that require reassessment by the nurse. These are typical characteristics of active labor contractions, which occur when the cervix dilates from 4 to 8 cm¹⁴. They do not indicate any complications or imminent delivery.
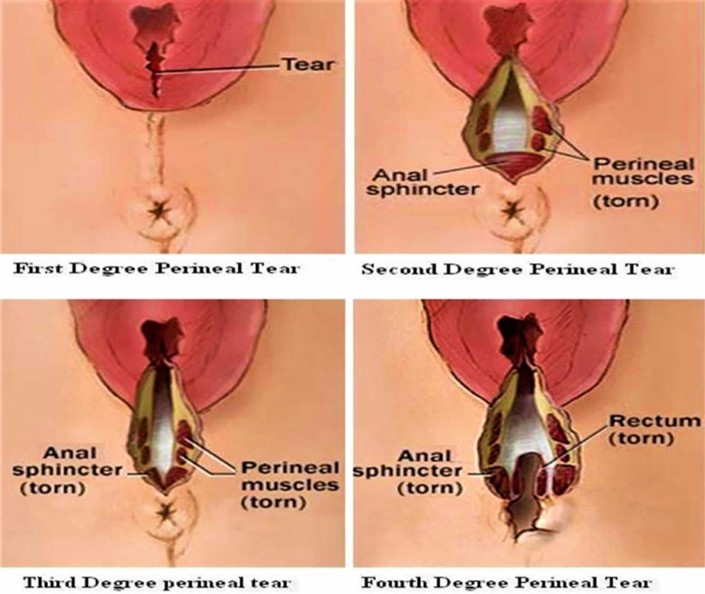
Correct Answer is D
Explanation
A fourth-degree laceration involves a tear that extends through the perineal muscles and extends to the anal sphincter. This type of laceration requires careful management to promote healing and prevent infection. Applying a moist, warm compress to the perineum helps to promote blood flow, reduce swelling, and provide comfort to the client.
Option a) Providing the client with a cool sitz bath is not appropriate for a fourth-degree laceration. Cool sitz baths are typically used for relieving discomfort and reducing swelling in cases of perineal trauma, but in the case of a fourth-degree laceration, warm compresses are preferred.
Option b) Administering methylergonovine 0.2 mg IM is not necessary for a fourth-degree laceration. Methylergonovine is a medication used to promote uterine contractions and prevent postpartum hemorrhage. However, it is not specifically indicated for the management of perineal lacerations.
Option c) Applying povidone-iodine to the client's perineum after she voids is not recommended for a fourth-degree laceration. Povidone-iodine is an antiseptic solution used to disinfect the skin. However, it is not typically used on open wounds, such as perineal lacerations, as it may delay wound healing.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
