A client with type 2 diabetes normally achieves adequate glycemic control through diet and exercise. Upon being admitted to the hospital for a cholecystectomy, however, the client has required insulin injections on two occasions. The nurse would identify what likely cause for this short-term change in treatment?
Stress has likely caused an increase in the client's blood sugar levels.
The client's volatile fluid balance surrounding surgery has likely caused unstable blood sugars.
The client has likely overstimulated her ability to control her diabetes using non-pharmacologic measures.
Alterations in bile metabolism and release have likely caused hyperglycemia.
The Correct Answer is A
A. Stress has likely caused an increase in the client's blood sugar levels:
This statement is accurate. Stress, especially related to surgery, can lead to increased levels of stress hormones, such as cortisol and catecholamines, which can elevate blood sugar levels. Surgery is a physiological stressor that can impact glucose metabolism.
B. The client's volatile fluid balance surrounding surgery has likely caused unstable blood sugars:
This is the most appropriate choice. Surgery, anesthesia, and changes in fluid balance can affect blood glucose levels. The stress response to surgery can lead to fluctuations in blood sugar, and patients may need insulin during this period.
C. The client has likely overstimulated her ability to control her diabetes using non-pharmacologic measures:
This statement is not accurate. Overstimulation is not a common cause of the need for insulin in the context of surgery. The stress and physiological changes associated with surgery are more likely contributors.
D. Alterations in bile metabolism and release have likely caused hyperglycemia:
While alterations in metabolism can impact glucose regulation, in the context of surgery, the primary factors are the stress response, changes in fluid balance, and potential alterations in the ability to eat or drink normally rather than specific effects on bile metabolism.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["B","C","E"]
Explanation
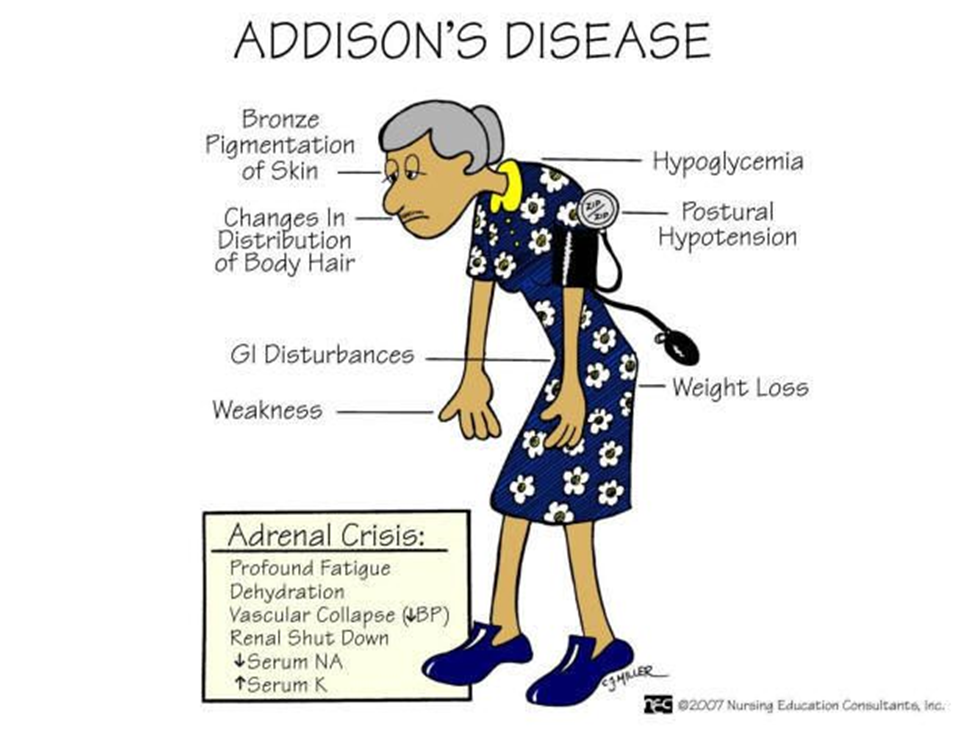
A. Buffalo hump:
Explanation: A buffalo hump is associated with excess cortisol, which is not a typical manifestation of Addison's disease. Instead, patients with Addison's disease may experience weight loss and muscle wasting.
B. Hyponatremia:
Explanation: Correct. Hyponatremia (low sodium levels) can occur in Addison's disease due to the loss of aldosterone, which plays a role in sodium and water balance.
C. Decreased glucose level:
Explanation: Correct. Addison's disease can lead to hypoglycemia (low blood glucose levels) because cortisol, which is important for maintaining blood glucose, is deficient.
D. Weight gain:
Explanation: Weight gain is not a typical manifestation of Addison's disease. Instead, weight loss and muscle wasting may occur.
E. Craving for salt:
Explanation: Correct. Addison's disease can lead to salt craving, as aldosterone deficiency results in increased sodium loss and potassium retention.
Correct Answer is A
Explanation
A. Metabolic Alkalosis:
pH: Elevated (alkalotic).
PaCO2: Normal or slightly decreased (compensation may or may not be present).
HCO3: Elevated.
Explanation: Metabolic alkalosis is characterized by an excess of bicarbonate (HCO3) in the blood, leading to an elevated pH. In this case, the elevated pH and HCO3 levels suggest that the primary imbalance is metabolic alkalosis.
B. Respiratory Alkalosis:
pH: Elevated (alkalotic).
PaCO2: Decreased (due to hyperventilation, which blows off CO2).
HCO3: Normal or slightly decreased (compensation).
Explanation: Respiratory alkalosis is characterized by low levels of carbon dioxide (PaCO2) due to hyperventilation. However, in the provided ABG, the PaCO2 is not significantly decreased, suggesting that respiratory alkalosis is not the primary issue.
C. Respiratory Acidosis:
pH: Decreased (acidotic).
PaCO2: Increased (due to inadequate ventilation).
HCO3: Normal or slightly elevated (compensation).
Explanation: Respiratory acidosis is characterized by an increase in carbon dioxide (PaCO2) levels. In this case, the PaCO2 is within the normal range, indicating that respiratory acidosis is not the primary problem.
D. Metabolic Acidosis:
pH: Decreased (acidotic).
PaCO2: Normal or slightly decreased (compensation).
HCO3: Decreased.
Explanation: Metabolic acidosis is characterized by a decrease in bicarbonate (HCO3) levels. In this ABG, the HCO3 is elevated, ruling out metabolic acidosis as the primary issue.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
