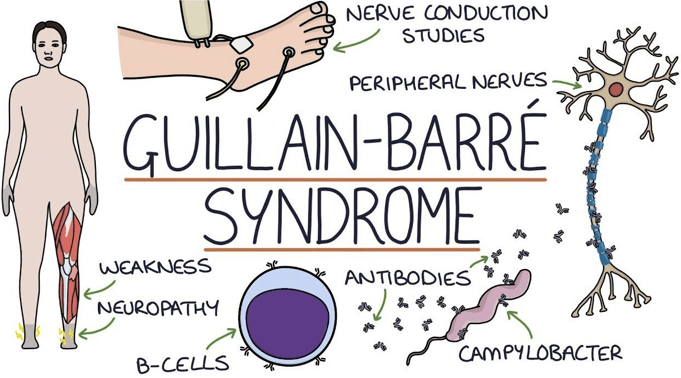
While caring for a client with Guillain-Barre syndrome, which finding should the practical nurse (PN) report to the charge nurse?
Irregular heart rate.
Profuse diaphoresis.
Lower leg weakness.
Full facial flushing.
The Correct Answer is A
This is the finding that the PN should report to the charge nurse because it indicates a possible complication of Guillain-Barre syndrome, which is autonomic dysfunction. This can affect the cardiac, respiratory, and gastrointestinal systems and cause life-threatening problems such as arrhythmias, hypotension, or respiratory failure. The PN should monitor the client's vital signs closely and report any abnormal changes.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
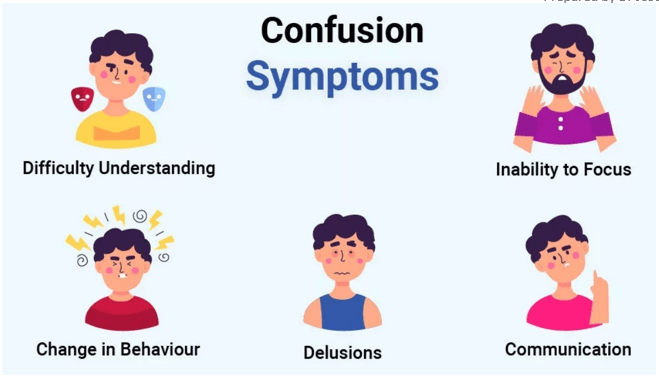
Correct Answer is C
Explanation
it provides reality orientation and helps the client cope with the change in environment. The client may be experiencing acute confusion or delirium due to stress, medication, infection, or other factors. The PN should remind the client of the date, time, and place frequently and use other strategies such as calendars, clocks, and familiar objects to reduce confusion.
Correct Answer is D
Explanation
A) Incorrect- While the history of vomiting is important to assess, it may not be the most crucial information to gather at this point, as the client is postoperative and the focus is on immediate postoperative care.
B) Incorrect- While assessing for fluid intake is important, the client's refusal of ice chips is not an urgent concern compared to other potential complications, such as pain management, oxygenation, and fluid balance.
C) Incorrect- These assessments are important, but the client's history of right hemicolectomy and the current infusion and medication administration require closer attention to fluid balance, pain control, and oxygenation.
D) Correct- While all options are important to consider, the most critical information in this scenario is assessing peripheral pulses and the range of motion of both legs. A right hemicolectomy involves abdominal surgery and decreased or absent peripheral pulses along with a limited range of motion could indicate impaired circulation, thrombosis, or other post-operative complications. These findings might necessitate prompt intervention to prevent potential complications.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
