The practical nurse (PN) is monitoring the neurological vital signs of a client with a recently closed head injury. Which vital sign trends indicate increased intracranial pressure (ICP) and should be reported to the charge nurse?
Heart rate above 110 beats/minute, elevated respiratory rate, and hypotension.
Bounding pulse rate, groaning respiratory effort, and elevated blood pressure.
Thready rapid pulse, trembling, perspiration, weakness, and irritability.
Bradycardia, irregular respiratory patterns, widening pulse pressure.
The Correct Answer is D
The vital sign trends that indicate increased intracranial pressure (ICP) and should be reported to the charge nurse are:
Bradycardia: A slow heart rate can be a sign of increased ICP.
Irregular respiratory patterns: Abnormal breathing patterns, such as irregular or Cheyne-Stokes respirations, can be indicative of increased ICP.
Widening pulse pressure: An increased difference between systolic and diastolic blood pressure (widening pulse pressure) can be a sign of increased ICP.
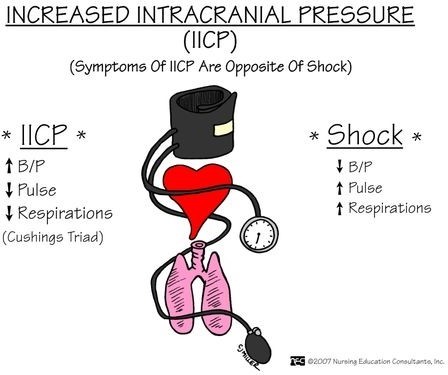
A- Heart rate above 110 beats/minute, elevated respiratory rate, and hypotension: While an elevated heart rate and respiratory rate can be associated with increased ICP, hypotension (low blood pressure) is not typically seen in this condition. Hypotension can be a sign of other factors, such as hypovolemia or shock, which may or may not be related to the head injury.
B- Bounding pulse rate, groaning respiratory effort, and elevated blood pressure: Bounding pulse rate and elevated blood pressure are not specific to increased ICP. They can be influenced by other factors such as pain, anxiety, or medications. Groaning respiratory effort may indicate respiratory distress, but it is not directly related to increased ICP.
C- Thready rapid pulse, trembling, perspiration, weakness, and irritability: These signs and symptoms can be associated with various conditions such as anxiety, stress, or other physiological responses. While they may occur in the context of increased ICP, they are not specific to this condition alone.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
To prevent injury in a female client with immune thrombocytopenic purpura (ITP) who is transferred to a long-term care facility for physical rehabilitation, the most important action for the practical nurse to implement is to ensure the client has minimal clutter in the room.
ITP is a condition characterized by a low platelet count, which can result in an increased risk of bleeding and bruising. Clutter in the room can pose a hazard and increase the risk of injury. The client may accidentally bump into objects or trip over items, potentially leading to falls or injuries.
Incorrect:
A- Assessing the client for nerve pain or paralysis is important but may not be directly related to preventing injury in this context. It is essential to address these concerns but not the most important action in preventing injury.
C- Evaluating the client's neurological status after exercising is important for overall assessment and monitoring but does not specifically address the prevention of injury.
D- Monitoring the client's blood cell laboratory values is essential for managing the client's condition but does not directly address preventing injury. It focuses more on the medical management of the client's ITP.
Correct Answer is C
Explanation
When assessing an older client with left-sided heart failure (HF), the most important intervention for the practical nurse (PN) to implement is to auscultate all lung fields. Left-sided heart failure is characterized by the inability of the left ventricle to effectively pump blood, leading to fluid accumulation in the lungs. Auscultating all lung fields allows the PN to assess for the presence of abnormal lung sounds such as crackles, indicating pulmonary congestion.
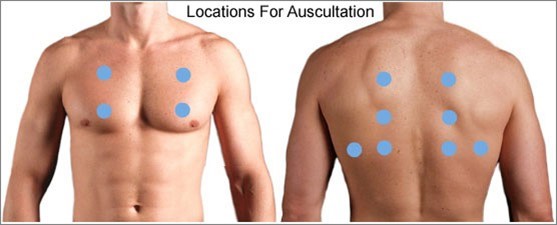
In summary, when assessing an older client with left-sided heart failure, the most important intervention for the practical nurse (PN) to implement is to auscultate all lung fields. This allows for the detection of abnormal lung sounds associated with pulmonary congestion, a hallmark sign of left-sided heart failure.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
