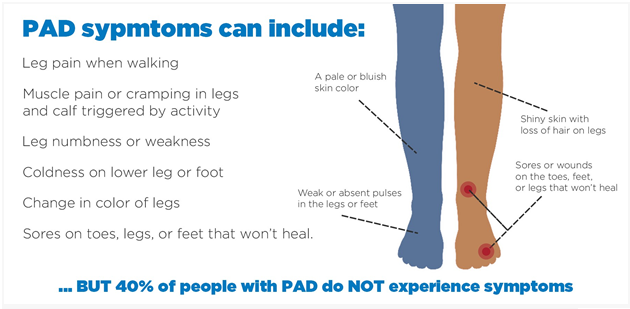
The nurse is teaching a client with peripheral arterial disease. Which information should the nurse include in the teaching plan?
Soak feet in warm water for an hour each day
Set heating pads on a low temperature.
Use callus remover for corns or calluses
Wear fitted closed toe shoes daily.
The Correct Answer is D
Wear fitted closed toe shoes daily: It is important for clients with peripheral arterial disease to wear properly fitted closed toe shoes. This helps protect the feet from injury and provides support. Closed toe shoes also help maintain warmth and prevent heat loss, which is especially important for individuals with impaired circulation.
Let's review the other options and explain why they may not be appropriate:
Soak feet in warm water for an hour each day: Soaking the feet in warm water for a prolonged period can actually worsen symptoms in individuals with peripheral arterial disease. It can cause further dilation of blood vessels, leading to increased blood pooling and potential tissue damage. Therefore, soaking the feet for extended periods of time is not recommended.
Set heating pads on a low temperature: Using heating pads, especially at high temperatures, can be harmful to individuals with peripheral arterial disease. It can increase the risk of burns or thermal injury due to reduced sensation in the affected areas. Heating pads should be used with caution and on a low temperature setting, if necessary.
Use callus remover for corns or calluses: Individuals with peripheral arterial disease have reduced blood flow to the lower extremities, which can impair wound healing. It is important to avoid self-treatment of corns or calluses, as it can increase the risk of skin breakdown and infection. Clients should be advised to consult a healthcare professional, such as a podiatrist, for appropriate management of corns and calluses.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
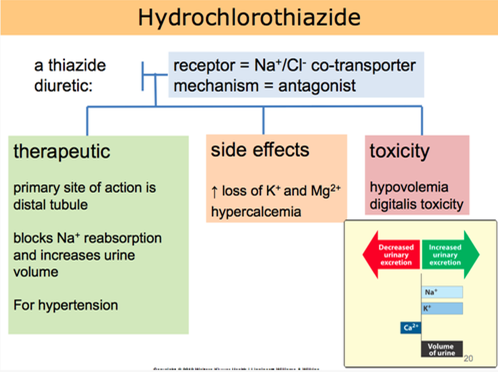
Hydrochlorothiazide is a diuretic medication commonly prescribed for hypertension. It works by increasing urine output, which helps to reduce fluid volume and lower blood pressure. Taking the medication in the morning is beneficial because the increased urine production during the day can help prevent nighttime disruptions due to frequent urination.
Let's go through the other statements and explain why they are not accurate:
"I will not take this medicine when my blood pressure is okay":
This statement indicates a misunderstanding about the purpose of hydrochlorothiazide. It is important to take prescribed medications consistently, even when blood pressure readings are within the normal range, as they are intended to help maintain blood pressure control.
"I will check blood pressure in both arms and legs before taking the drug":
Checking blood pressure in both arms and legs is not directly related to hydrochlorothiazide use. Blood pressure should be monitored regularly, but it is not necessary to perform these measurements specifically before taking the medication.
"I will decrease potassium foods such as bananas in my diet":
Hydrochlorothiazide can cause potassium loss as a side effect. However, reducing potassium-rich foods without healthcare provider guidance may not be appropriate. It is important for the client to discuss dietary adjustments and potassium supplementation with their healthcare provider if needed.
Correct Answer is A
Explanation
The best response by the nurse would be to explain that no food or drink is allowed for 4 hours before the stress test.
The reason for this restriction is that consuming food or drink can affect the accuracy of the cardiac stress test results. Eating or drinking can increase heart rate and blood pressure, potentially altering the test's interpretation. It is important for the client to have an empty stomach to ensure accurate test results.
Let's review the other options and explain why they are not the best responses:
Asking the client's visitor to bring some coffee from the cafeteria for the client: This option goes against the restriction of no food or drink before the stress test. It is important to adhere to the guidelines provided to ensure accurate test results.
Making up a small breakfast tray from what is available on the unit: Similarly, providing breakfast to the client goes against the restriction of no food before the stress test. The client should have an empty stomach for the test.
Offering hot tea or coffee only: While hot tea or coffee might be tempting for the client, it still violates the requirement of no food or drink before the stress test. The client should only be allowed to consume water during the fasting period.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
