The nurse is conducting client teaching about cholesterol levels. When discussing the client's elevated LDL and lowered HDL levels, the client shows an understanding of the significance of these levels by making what statement?
"Increased LDL and decreased HDL increase my risk of coronary artery disease."
"Increased LDL has the potential to decrease my risk of heart disease."
"The decreased HDL level will increase the amount of cholesterol moved away from the artery walls."
"The increased LDL will decrease the amount of cholesterol deposited on the artery walls."
The Correct Answer is A
Elevated levels of LDL (low-density lipoprotein) cholesterol are associated with an increased risk of coronary artery disease (CAD). LDL cholesterol is often referred to as "bad" cholesterol because it can contribute to the formation of plaque in the arteries, leading to narrowing and blockage of the arteries supplying the heart. This increases the risk of developing CAD and related complications such as heart attack and stroke.
On the other hand, HDL (high-density lipoprotein) cholesterol is often referred to as "good" cholesterol. HDL cholesterol helps remove excess cholesterol from the bloodstream and transport it back to the liver for processing and excretion. Higher levels of HDL cholesterol are associated with a decreased risk of CAD because it helps to prevent the accumulation of cholesterol on artery walls.
Therefore, understanding that increased LDL and decreased HDL levels increase the risk of coronary artery disease demonstrates a good understanding of the significance of cholesterol levels and their impact on cardiovascular health.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
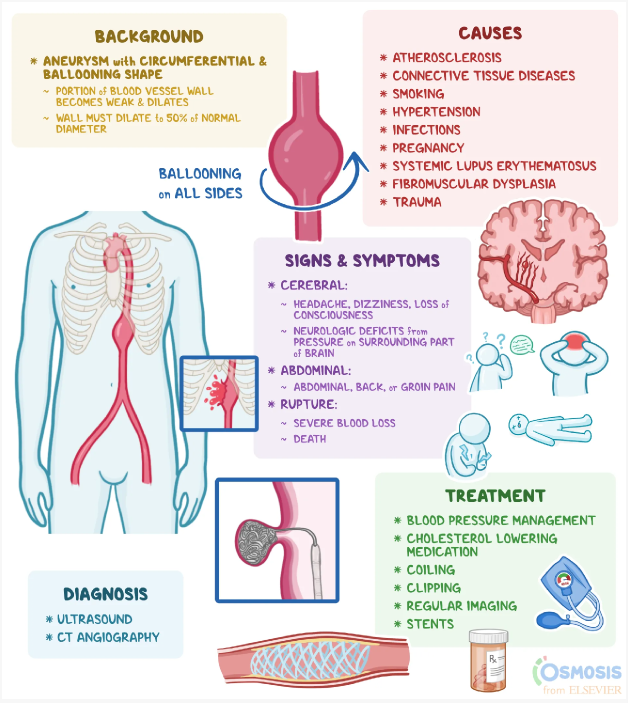
Abdominal aortic aneurysms (AAA) often do not present with specific symptoms in the early stages. It is not uncommon for individuals with AAA to be asymptomatic or have vague symptoms. Therefore, the absence of abdominal pain or any problems related to the abdomen is a common finding during the assessment of a client with an abdominal aortic aneurysm.
Let's briefly review the other statements:
"I have stomach pain every time I eat a big, heavy meal": This statement is more suggestive of gastrointestinal issues such as indigestion or acid reflux rather than specifically related to an abdominal aortic aneurysm.
"I have periodic episodes of constipation and then diarrhea": This statement may indicate gastrointestinal issues, but it is not a typical symptom associated with an abdominal aortic aneurysm. AAA is primarily related to the aorta, the main blood vessel in the abdomen, and its symptoms are not directly linked to bowel function.
"I belch a lot, especially when I lay down after eating": This statement suggests gastrointestinal symptoms such as acid reflux or gastroesophageal reflux disease (GERD). While these symptoms may be unrelated to the abdominal aortic aneurysm itself, they can coexist with other conditions.
Correct Answer is A
Explanation
The best response by the nurse would be to explain that no food or drink is allowed for 4 hours before the stress test.
The reason for this restriction is that consuming food or drink can affect the accuracy of the cardiac stress test results. Eating or drinking can increase heart rate and blood pressure, potentially altering the test's interpretation. It is important for the client to have an empty stomach to ensure accurate test results.
Let's review the other options and explain why they are not the best responses:
Asking the client's visitor to bring some coffee from the cafeteria for the client: This option goes against the restriction of no food or drink before the stress test. It is important to adhere to the guidelines provided to ensure accurate test results.
Making up a small breakfast tray from what is available on the unit: Similarly, providing breakfast to the client goes against the restriction of no food before the stress test. The client should have an empty stomach for the test.
Offering hot tea or coffee only: While hot tea or coffee might be tempting for the client, it still violates the requirement of no food or drink before the stress test. The client should only be allowed to consume water during the fasting period.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
