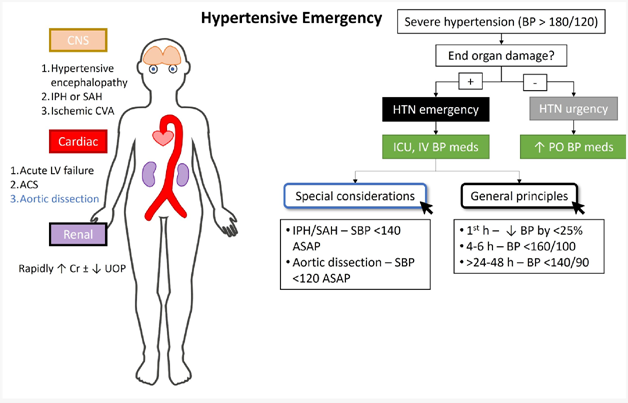
The nurse is assessing a client with a hypertensive emergency. Which finding is most important to report to the health care provider?
The client reports a headache with pain at level 5 of 10
The client has epistaxis after blowing his nose several times
The client has a urine output of 120 mL over a 4 hours
The client has a new-onset blurry vision and facial asymmetry
The Correct Answer is D
The client reports a headache with pain at level 5 of 10.: While a headache can be a symptom of high blood pressure, a pain level of 5 out of 10 alone does not indicate an immediate life-threatening condition. It is important to assess and manage the client's pain, but it may not be the most critical finding to report in this situation.
The client has epistaxis after blowing his nose several times. : Epistaxis, or a nosebleed, can occur due to high blood pressure, but it is not the most urgent or critical symptom in a hypertensive emergency. While it is essential to address the nosebleed and monitor blood pressure, other symptoms may indicate more severe consequences of uncontrolled high blood pressure.
The client has a urine output of 120 mL over 4 hours.: While decreased urine output can be a concerning sign, it is not the most significant finding to report in a hypertensive emergency. In this scenario, the focus is on acute complications related to high blood pressure, such as organ damage or impending stroke, which require immediate attention.
In summary, the finding that is most important to report to the healthcare provider in a client with a hypertensive emergency is the presence of new-onset blurry vision and facial asymmetry. These symptoms suggest potential neurological involvement and the need for urgent medical intervention to prevent serious complications like stroke.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
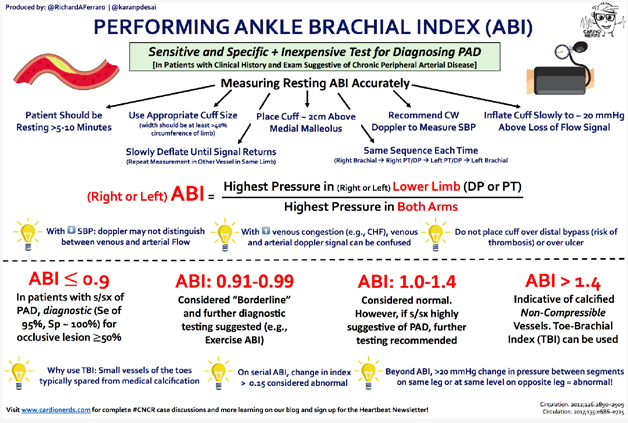
Correct Answer is C
Explanation
Based on the information provided, an Ankle-Brachial Index (ABI) of 0.89 indicates a mild reduction in blood flow to the lower extremities, suggesting peripheral arterial disease (PAD). In this case, the nurse should educate the client about the use of compression stockings.
Compression stockings are a conservative management approach for peripheral arterial disease. They help improve blood flow and alleviate symptoms by applying pressure to the legs, promoting venous return, and reducing swelling. Educating the client about the use of compression stockings can help improve circulation and manage symptoms such as pain, cramping, and fatigue.
Let's review the other options and explain why they are not the most appropriate interventions in this scenario:
Document the information as a normal finding: An ABI of 0.89 indicates an abnormal finding suggestive of peripheral arterial disease. It should not be documented as a normal finding, as it requires further assessment and intervention.
Prepare the client for an arterial bypass: An arterial bypass is a surgical intervention that is typically reserved for more severe cases of peripheral arterial disease. With an ABI of 0.89, which indicates mild reduction in blood flow, arterial bypass is not the first-line intervention. Conservative measures and medical management are usually recommended initially.
Anticipate a prescription for clopidogrel and simvastatin: Medications like clopidogrel (antiplatelet) and simvastatin (statin) may be prescribed for peripheral arterial disease. However, the next appropriate step after obtaining an ABI of 0.89 would be to educate the client about the use of compression stockings as a conservative management option before considering medication therapy.
Correct Answer is C
Explanation
The inability to move the left arm and leg suggests a neurological deficit, which is a significant finding that requires immediate attention. It could indicate a potential stroke or another neurological emergency that requires prompt evaluation and intervention. The health care provider needs to be notified immediately so that appropriate diagnostic tests and interventions can be initiated.
Tremors in the fingers when extending the arms can be a sign of tremor disorders or medication side effects but may not warrant immediate intervention.
Atrial fibrillation is a cardiac arrhythmia that requires monitoring and management but may not be directly related to the acute neurological issue.
The headache reported by the patient, although significant, is subjective and may be related to the hypertensive emergency or other factors but does not require immediate intervention compared to the potential neurological deficit.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
