The nurse is assessing a client with a presumptive diagnosis of peripheral arterial disease. The nurse obtains an Ankle-Brachial index of 0.89. Which intervention should the nurse take next?
Document the information as a normal finding
Prepare the client for an arterial bypass
Educate the client about the use of compression stocking
Anticipate a prescription for clopidogrel and simvastatin
The Correct Answer is D
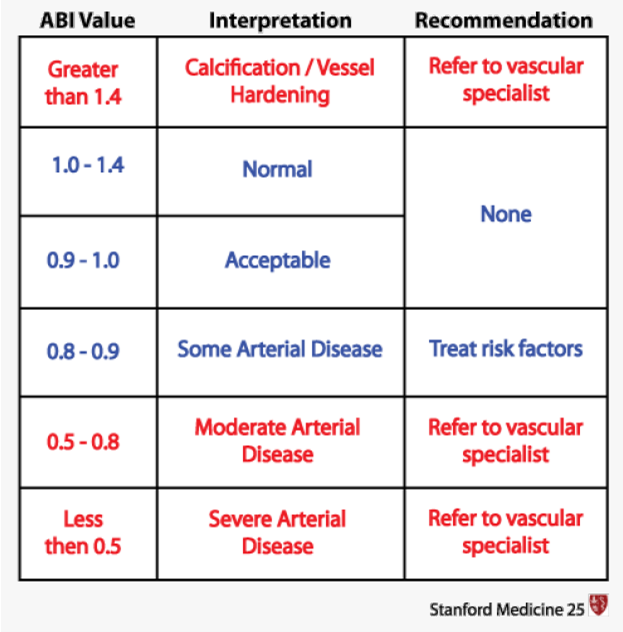
An ABI of 0.89 indicates a reduced blood flow to the lower extremities, which is suggestive of peripheral arterial disease (PAD). In PAD, there is narrowing or blockage of the arteries that supply blood to the legs and feet. Medications like clopidogrel and simvastatin are commonly prescribed for individuals with PAD to manage the condition and reduce the risk of complications.
Here's an explanation of why the other options are not the most appropriate interventions:
Document the information as a normal finding: An ABI of 0.89 is not considered a normal finding. An ABI value below 0.9 is generally indicative of PAD or reduced blood flow to the lower extremities.
Prepare the client for an arterial bypass: An ABI value of 0.89 alone does not warrant immediate preparation for an arterial bypass. Arterial bypass surgery is typically considered for severe cases of PAD with significant symptoms that significantly impact the client's quality of life and other conservative treatments have not been successful.
Educate the client about the use of compression stockings: While compression stockings may be a part of the overall management of PAD, the ABI result alone does not indicate an immediate need for education about compression stockings. Other interventions, such as medication management, lifestyle modifications, and possibly revascularization procedures, may be more appropriate based on the severity of the PAD.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["A","B","C","D"]
Explanation
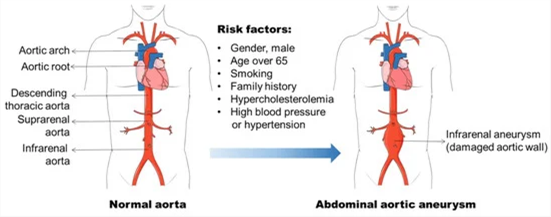
The information that the nurse should include in the discharge teaching for the client who is three days post-operative abdominal aortic aneurysm repair is as follows:
Notify the healthcare provider (HCP) of any redness or irritation of the incision: This is important because redness or irritation can be signs of infection or other complications at the surgical site. Prompt reporting allows for early intervention and management.
Do not lift anything more than 20 pounds: Following abdominal aortic aneurysm repair, it is crucial to avoid heavy lifting or straining as it can put excessive pressure on the surgical site and potentially lead to complications such as incisional hernia. Restricting lifting to no more than 20 pounds helps to protect the incision and promote proper healing.
Inform the client that there may be pain not relieved with pain medication: Pain management is an essential aspect of post-operative care. However, it is important for the client to understand that complete relief of pain may not always be achievable with pain medication alone. They should be aware that mild to moderate discomfort may persist during the healing process, but severe or worsening pain should be reported to the healthcare provider.
Stress the importance of having daily bowel movements: After abdominal surgery, it is common for bowel movements to be delayed due to factors such as anesthesia, reduced activity, and pain medication. However, it is crucial for the client to maintain regular bowel movements to prevent constipation and potential complications such as bowel obstruction. The nurse should provide guidance on strategies to promote regular bowel function, such as staying hydrated, eating a balanced diet rich in fiber, and using stool softeners or gentle laxatives as directed by the healthcare provider.
Correct Answer is D
Explanation
The nurse should prioritize notifying the surgeon and anesthesiologist as the first action. The absent pulses, coolness, and mottled appearance of the leg indicate potential compromised blood flow to the lower extremity, which could be a sign of vascular compromise or acute limb ischemia. These findings are concerning after the repair of an abdominal aortic aneurysm and require immediate medical attention.
Wrap both legs in a warming blanket: While it is important to maintain the client's body temperature, this action alone may not address the underlying issue of compromised blood flow and potential limb ischemia. Notifying the surgeon and anesthesiologist is the priority to address the immediate concern.
Compare findings to the preoperative assessment of the pulses: While comparing findings to the preoperative assessment is important for evaluating the client's condition, it should not delay immediate action. The priority in this situation is to promptly notify the surgeon and anesthesiologist to address the potential vascular compromise.
Document the findings and recheck in 15 minutes: Documenting the findings is an important step in the nursing process, but it should not take precedence over immediate intervention. The concerning signs of absent pulses, coolness, and mottled appearance require urgent attention, and delaying notification could lead to further complications.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
