A nurse is assessing a client with a history of high blood pressure. The client's blood pressure is 210/106 mm Hg during the assessment. What follow-up question should the nurse ask?
"Have you recently taken any antihistamines?"
"Have there been recent stressful events in your life?"
"Did you take any acetaminophen today?"
"Have you consistently taken your medications?"
The Correct Answer is D
Choice D: This question is crucial as it addresses the client's adherence to their prescribed medication regimen for managing high blood pressure. Consistent medication use is essential for controlling blood pressure and reducing the risk of complications associated with hypertension. The elevated blood pressure reading suggests that the current medication regimen may not be effectively controlling the client's blood pressure. By assessing medication adherence, the nurse can determine if non-adherence is contributing to the high blood pressure reading or if adjustments to the medication regimen are required.
"Have you recently taken any antihistamines?": Asking about recent antihistamine use is not directly relevant to the client's high blood pressure reading of 210/106 mm Hg. Antihistamines are medications primarily used to relieve allergy symptoms and do not typically have a significant impact on blood pressure levels.
"Have there been recent stressful events in your life?": While stress can contribute to temporary increases in blood pressure, asking about recent stressful events is not the most critical follow-up question in this situation. The client's blood pressure reading of 210/106 mm Hg indicates a severe elevation that requires immediate attention and management beyond stress reduction alone.
"Did you take any acetaminophen today?": Acetaminophen, also known as paracetamol, is a pain reliever and fever reducer. It does not typically have a significant effect on blood pressure. Therefore, asking about acetaminophen use is not the most relevant follow-up question for the client's high blood pressure reading.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
While it is generally recommended to avoid close or prolonged exposure to strong magnetic fields, such as those generated by MRI machines, placing items that generate magnetic fields over the pacemaker/ICD, such as cell phones or certain medical devices, does not typically pose a risk. Therefore, it would be important for the nurse to clarify the client's understanding and provide accurate information about the precautions related to magnetic fields.
The other statements made by the client are generally correct and align with the typical recommendations for individuals with pacemakers/ICDs:
Avoiding contact sports or lifting heavy objects for a specified period of time after pacemaker/ICD insertion is usually advised to allow for proper healing and to reduce the risk of lead dislodgment or damage to the device.
Informing dentists and healthcare providers about the presence of a pacemaker/ICD is important so that they can take appropriate precautions during procedures or treatments that may involve electromagnetic interference or interfere with the device's functioning.
While it is generally advised to avoid close proximity to strong magnetic fields, such as those in airports or certain household appliances, it does not necessarily mean completely avoiding them. The nurse can clarify the specific recommendations regarding metal detectors at airports and the safe use of household appliances.
Correct Answer is D
Explanation
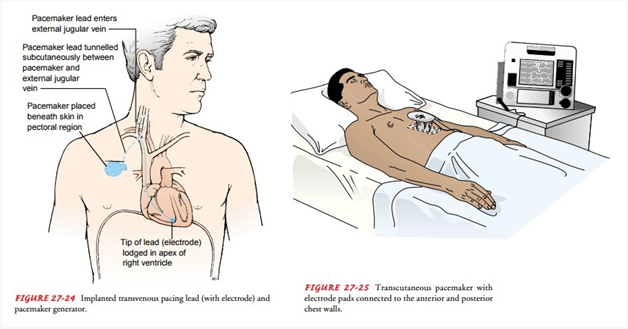
Sinus bradycardia with a heart rate of 32 beats/min and accompanying hypotension and symptoms of feeling faint indicates significant hemodynamic compromise. In such cases, the first-line intervention is to provide external cardiac pacing through transcutaneous pacemaker (TCP) pads. TCP can help increase the heart rate and improve cardiac output by delivering electrical impulses to the heart.
Administering the scheduled dose of diltiazem (Cardizem), a calcium channel blocker, is not appropriate in this situation. Diltiazem can further lower the heart rate and blood pressure, exacerbating the client's symptoms and potentially leading to adverse effects.
Repositioning the patient on the left side or having the patient perform the Valsalva maneuver are not effective interventions for treating sinus bradycardia with hemodynamic compromise. These actions may be used in specific situations, but in this case, the client requires immediate intervention to address the low heart rate and blood pressure.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
