A nurse accompanies a client to an exercise stress test. The client can achieve the target heart rate, but the electrocardiogram indicates ST-segment elevation. Which procedure will the nurse prepare the patient for?
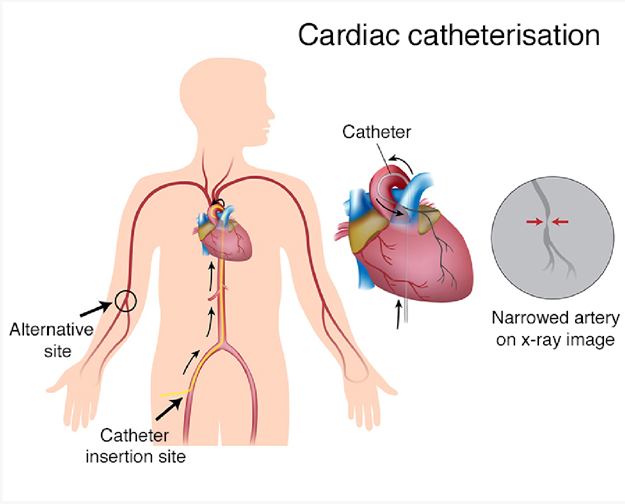
cardiac catheterization
transesophageal echocardiogram
telemetry monitoring
pharmacologic stress test
The Correct Answer is A
ST-segment elevation during exercise stress testing is a concerning finding that may indicate reduced blood flow to the heart muscle. It can be a sign of myocardial ischemia or coronary artery disease. Cardiac catheterization is a diagnostic procedure that allows direct visualization of the coronary arteries and helps identify any blockages or narrowing that may be causing the ST-segment elevation.
Here's an explanation of why the other options are not the most appropriate procedures:
Transesophageal echocardiogram: Transesophageal echocardiogram (TEE) is a diagnostic test that involves inserting a probe into the esophagus to obtain detailed images of the heart. It is not typically used to evaluate ST-segment elevation, which primarily indicates coronary artery issues rather than structural abnormalities.
Telemetry monitoring: Telemetry monitoring involves continuous monitoring of a patient's heart rhythm and can be used for various cardiac conditions. While telemetry monitoring may be necessary for ongoing cardiac assessment, it is not a specific procedure to address the ST-segment elevation found during the exercise stress test.
Pharmacologic stress test: A pharmacologic stress test is an alternative to an exercise stress test for patients who cannot exercise. It involves administering medications that stimulate the heart to mimic the effects of exercise. While a pharmacologic stress test can also reveal ST-segment changes, the presence of ST-segment elevation usually requires further evaluation with a more invasive procedure like cardiac catheterization.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Defibrillation is not the first-line treatment for atrial fibrillation. It is used to treat life-threatening cardiac arrhythmias such as ventricular fibrillation or pulseless ventricular tachycardia. Atrial fibrillation, on the other hand, is a rapid and irregular atrial rhythm, and defibrillation is not indicated for its treatment.
Obtain consent for transesophageal echocardiogram (TEE): This is an appropriate action for a client with atrial fibrillation. A TEE is often performed to assess the structure and function of the heart in cases of atrial fibrillation, especially when considering cardioversion or other interventions.
Obtain consent for cardioversion: Cardioversion is a common treatment option for atrial fibrillation, especially when the client is unstable or experiencing symptoms. It involves restoring a normal heart rhythm through the use of electrical shocks or medications. It is important to obtain informed consent before performing cardioversion, but this does not necessarily require questioning.
Hold digoxin 48 hours prior to cardioversion: Digoxin is commonly held before cardioversion because it can increase the risk of certain arrhythmias during the procedure. This is a standard precaution to minimize potential adverse effects. Therefore, the nurse does not need to question this action, as it aligns with established guidelines.
Correct Answer is C
Explanation
Maintaining a 2 gram-sodium (salt) diet is an important aspect of managing hypertension. High sodium intake can contribute to elevated blood pressure. Therefore, reducing sodium intake is recommended to help control blood pressure levels. The nurse should provide guidance on reading food labels, avoiding high-sodium processed foods, and incorporating a diet rich in fruits, vegetables, and whole grains.
The other options listed are not appropriate or beneficial for managing hypertension:
Maintaining a low-potassium diet: Potassium is an essential mineral that helps regulate blood pressure. While specific potassium restrictions may be necessary for some individuals with certain medical conditions, most people with hypertension do not need to limit their potassium intake. In fact, a balanced diet with adequate potassium is generally recommended.
Skipping a medication dose if dizziness occurs: It is not advisable to skip medication doses without consulting a healthcare provider. Hypertension medications are prescribed to help control blood pressure, and missing doses can lead to uncontrolled hypertension and potential complications. If the client experiences dizziness or other side effects from the medication, they should consult their healthcare provider for appropriate management.
Drinking three glasses of wine a day: Excessive alcohol consumption can contribute to elevated blood pressure. The recommended alcohol intake for individuals with hypertension is moderate or limited to moderate levels, which typically means no more than one drink per day for women and two drinks per day for men. Drinking excessive amounts of wine or any alcoholic beverage can negatively affect blood pressure control.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
