The nurse on the intermediate care unit received change-of-shift report on four clients with hypertension. Which patient should the nurse assess first?
A client with a blood pressure of 190/92 mm Hg who reports chest pain
A client with a blood pressure of 190/104 mm Hg who has sinus tachycardia
A client with a blood pressure of 178/90 mm Hg who has intermittent claudication
A client with a blood pressure of 172/98 mm Hg scheduled for a stress test
The Correct Answer is A
The nurse should assess the client with a blood pressure of 190/92 mm Hg who reports chest pain first. Chest pain can be a symptom of myocardial ischemia or a heart attack, which requires immediate attention. The combination of high blood pressure and chest pain is concerning and may indicate acute coronary syndrome. Prompt assessment and intervention are crucial to evaluate the cause of the chest pain and initiate appropriate treatment.
A client with a blood pressure of 190/104 mm Hg who has sinus tachycardia: While sinus tachycardia may indicate increased heart rate, it does not necessarily require immediate assessment unless other concerning symptoms are present. However, the nurse should address the elevated blood pressure in a timely manner.
Intermittent claudication refers to leg pain or discomfort during physical activity due to reduced blood flow. While it is important to assess and manage this symptom, it is not typically considered an urgent condition requiring immediate assessment compared to chest pain.
The client scheduled for a stress test may have elevated blood pressure, but if they are stable and not currently experiencing symptoms, they may not require immediate assessment compared to a client with chest pain.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
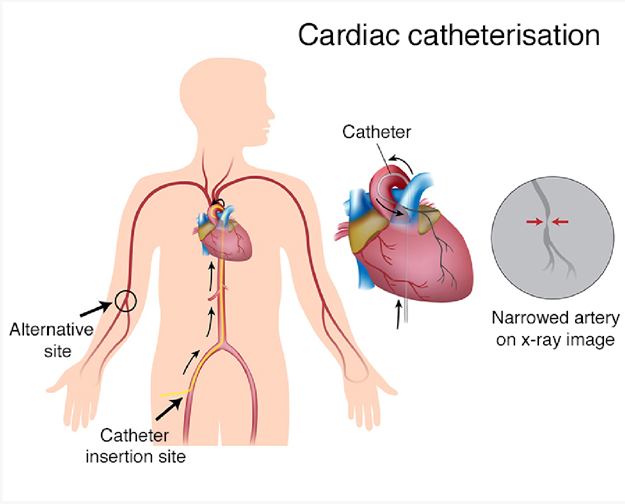
ST-segment elevation during exercise stress testing is a concerning finding that may indicate reduced blood flow to the heart muscle. It can be a sign of myocardial ischemia or coronary artery disease. Cardiac catheterization is a diagnostic procedure that allows direct visualization of the coronary arteries and helps identify any blockages or narrowing that may be causing the ST-segment elevation.
Here's an explanation of why the other options are not the most appropriate procedures:
Transesophageal echocardiogram: Transesophageal echocardiogram (TEE) is a diagnostic test that involves inserting a probe into the esophagus to obtain detailed images of the heart. It is not typically used to evaluate ST-segment elevation, which primarily indicates coronary artery issues rather than structural abnormalities.
Telemetry monitoring: Telemetry monitoring involves continuous monitoring of a patient's heart rhythm and can be used for various cardiac conditions. While telemetry monitoring may be necessary for ongoing cardiac assessment, it is not a specific procedure to address the ST-segment elevation found during the exercise stress test.
Pharmacologic stress test: A pharmacologic stress test is an alternative to an exercise stress test for patients who cannot exercise. It involves administering medications that stimulate the heart to mimic the effects of exercise. While a pharmacologic stress testcan also reveal ST-segment changes, the presence of ST-segment elevation usually requires further evaluation with a more invasive procedure like cardiac catheterization.
Correct Answer is C
Explanation
The most important finding to report to the health care provider would be the serum potassium level of 3.0 mEq. This is an extremely low potassium level (normal range is typically 3.5-5.0 mEq/L), which can indicate a potentially life-threatening condition called hypokalemia. Furosemide (Lasix) is a diuretic medication that can cause potassium loss in the urine, and a low potassium level can lead to serious cardiac and muscle abnormalities. It is crucial to report this finding promptly to the health care provider for appropriate intervention and monitoring.
Blood glucose level of 175 mg/dL: While an elevated blood glucose level can be a concern, especially for individuals with diabetes, it is not the most critical finding in this situation. The client's primary concern is hypertension, and the administration of IV furosemide is aimed at managing blood pressure. The elevated blood glucose level should still be addressed and monitored, but it is not as urgent as the low potassium level.
Orthostatic systolic BP decrease of 12 mm Hg: Orthostatic hypotension refers to a significant decrease in blood pressure upon standing up. While it is important to assess and manage orthostatic changes, a decrease of 12 mm Hg in systolic blood pressure alone may not be considered clinically significant. It could be a normal response for some individuals. However, if the client experiences symptoms such as dizziness or lightheadedness upon standing, further evaluation may be necessary. Nonetheless, it is not as urgent as the low potassium level.
Current blood pressure reading of 166/94 mm Hg: While this blood pressure reading indicates hypertension, it is not the most critical finding to report in this situation. The nurse is preparing to administer furosemide (Lasix), which is a medication commonly used to treat hypertension. It is expected that the blood pressure will be high before administering the medication. The goal is to monitor the blood pressure after the administration to assess the effectiveness of the medication.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
