The nurse and unlicensed assistive personnel (UAP) on the telemetry unit are caring for four clients. Which nursing action can be delegated to the UAP?
Checking the client's catheter site after a coronary angiogram
Teaching a patient about exercise electrocardiography
Attaching ECG monitoring electrodes after a patient bathes
Monitoring a client after a transesophageal echocardiogram
The Correct Answer is D
Monitoring a client after a transesophageal echocardiogram involves observing the client for any immediate post-procedure complications or adverse reactions. This may include assessing vital signs, monitoring for signs of bleeding or infection, and reporting any concerning symptoms or changes in the client's condition to the nurse.
Checking the client's catheter site after a coronary angiogram requires assessing the site for bleeding, hematoma, or signs of infection. This task involves more complex assessment skills and would typically be performed by the nurse.
Teaching a patient about exercise electrocardiography involves providing education on the purpose of the test, the procedure itself, and any preparation or precautions the patient needs to take. This task requires specialized knowledge and is best performed by the nurse who can address the patient's specific questions and concerns.
Attaching ECG monitoring electrodes after a patient bathes requires technical knowledge and skill in properly placing the electrodes and ensuring accurate ECG readings. This task also falls within the scope of the nurse's responsibilities.
Delegation should be based on the UAP's skill set, training, and the complexity of the task. While the UAP can provide valuable support in monitoring a client after a transesophageal echocardiogram, the other tasks mentioned require the expertise and knowledge of a nurse.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
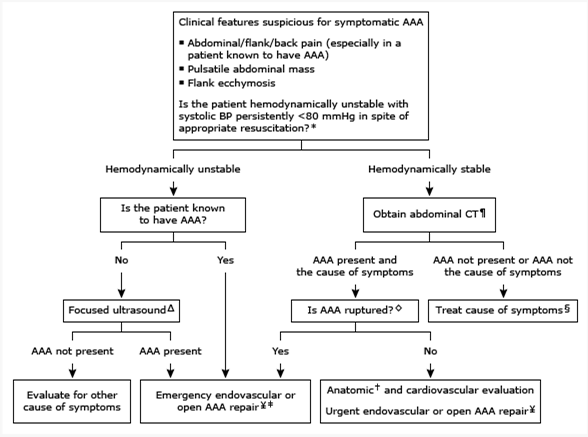
Based on the information provided, the nurse should anticipate that the medical treatment prescribed for a client with an abdominal aortic aneurysm less than 3 cm in size would be regular ultrasound screenings every six (6) months.
Monitoring the size of the abdominal aortic aneurysm through ultrasound is a common approach for managing small aneurysms. Regular ultrasound screenings allow healthcare providers to track the growth rate of the aneurysm and determine if any intervention, such as surgical repair, is necessary as the aneurysm progresses in size.
Let's review the other options and explain why they are not the most appropriate treatments for an abdominal aortic aneurysm less than 3 cm in size:
Intravenous pyelogram yearly: An intravenous pyelogram is an imaging test used to evaluate the urinary system, specifically the kidneys, ureters, and bladder. It is not directly related to the management or monitoring of an abdominal aortic aneurysm.
Assessment of abdominal girth monthly: Assessing the abdominal girth may be a part of the overall assessment of the client's condition, but it is not the primary treatment for managing an abdominal aortic aneurysm. Monitoring the aneurysm size through regular ultrasound screenings is a more specific and accurate approach.
Repair of abdominal aortic aneurysm: Repair of an abdominal aortic aneurysm is typically indicated when the aneurysm reaches a certain size threshold or if it poses a high risk of rupture. For an aneurysm less than 3 cm in size, repair is usually not the initial treatment option. Instead, regular monitoring through ultrasound screenings is recommended to assess the aneurysm's growth rate and determine the appropriate time for intervention.
Correct Answer is ["A","C","D","E"]
Explanation
The questions related to the client's history that are most important to ask are:
How would you describe your symptoms?: This question is important to assess the client's current cardiac symptoms and determine the severity, duration, and nature of their symptoms. It helps the nurse to evaluate the client's cardiac status and determine appropriate interventions.
Are you allergic to any medications or foods?: This question is crucial to identify any potential allergies that could impact the client's cardiac care. It helps the nurse ensure that medications and interventions are safe for the client and prevent any adverse reactions.
How did your mother die?:This question is important to gather information about the client's family history of cardiac diseases and potential risk factors. Understanding the family history helps the nurse assess the client's genetic predisposition to cardiac conditions and plan appropriate interventions and screenings.
Have you had shortness of breath or weight gain? : This question is important to assess for symptoms of heart failure or fluid retention. Shortness of breath and weight gain can indicate fluid accumulation, which is a common symptom in cardiac conditions. It helps the nurse evaluate the client's cardiac function and determine the need for furtherinterventions or medication adjustments.
Let's review the other options and explain why they are not the most important questions to ask:
Do you have any children?: While family history is important, specifically asking about children is not as relevant to the client's current cardiac condition. The focus should be on the client's own symptoms, medical history, and family history of cardiac diseases.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
