The nurse is caring for a client scheduled for a cardiac stress test at 1100. When the nurse enters the client's room at 0800, the client requests toast or at least some coffee. What is the best response?
Explain that no food or drink is allowed for 4 hours before the stress test.
Ask the client's visitor to bring some coffee from the cafeteria for the client.
Make up a small breakfast tray from what is available on the unit.
Offer hot tea or coffee only.
The Correct Answer is A
The best response by the nurse would be to explain that no food or drink is allowed for 4 hours before the stress test.
The reason for this restriction is that consuming food or drink can affect the accuracy of the cardiac stress test results. Eating or drinking can increase heart rate and blood pressure, potentially altering the test's interpretation. It is important for the client to have an empty stomach to ensure accurate test results.
Let's review the other options and explain why they are not the best responses:
Asking the client's visitor to bring some coffee from the cafeteria for the client: This option goes against the restriction of no food or drink before the stress test. It is important to adhere to the guidelines provided to ensure accurate test results.
Making up a small breakfast tray from what is available on the unit: Similarly, providing breakfast to the client goes against the restriction of no food before the stress test. The client should have an empty stomach for the test.
Offering hot tea or coffee only: While hot tea or coffee might be tempting for the client, it still violates the requirement of no food or drink before the stress test. The client should only be allowed to consume water during the fasting period.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["D","E"]
Explanation
The traces that should require immediate follow-up by the nurse are:
● Pacer spikes occur directly before the T waves.
Pacer spikes occurring on the T waves indicate an issue with the pacemaker's timing or sensing. This could lead to inappropriate pacing or pacing during the refractory period, which can be detrimental to the client's heart function.
● The heart rate is outside of programmed parameters.
If the heart rate is outside of the programmed parameters set for the client's pacemaker, it may indicate a malfunction or failure of the device or a change in the client's cardiac status. It is important for the nurse to assess the client's condition and notify the healthcare provider for further evaluation and intervention.
Let's review the other options and explain why they do not require immediate follow-up:
Pacer spikes are adequate in number: This indicates that the pacemaker is delivering the appropriate number of electrical impulses as programmed. As long as the other parameters are normal, this finding does not require immediate follow-up.
Pacer spikes occur directly before the P waves: This is the desired and expected pattern for a pacemaker in normal sinus rhythm. It indicates proper timing and coordination between the pacemaker and the client's intrinsic electrical activity.
Pacer spikes occur directly before the QRS waves: This is also the desired and expected pattern for a pacemaker in clients with ventricular pacing. It indicates proper timing and coordination between the pacemaker and the client's intrinsic electrical activity.
The heart rate is within programmed parameters: If the heart rate falls within the programmed parameters set for the client's pacemaker, it indicates that the device is functioning appropriately in maintaining the desired heart rate.
Correct Answer is D
Explanation
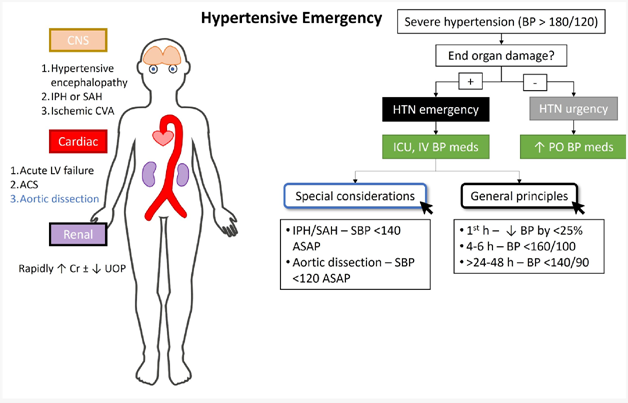
The client reports a headache with pain at level 5 of 10.: While a headache can be a symptom of high blood pressure, a pain level of 5 out of 10 alone does not indicate an immediate life-threatening condition. It is important to assess and manage the client's pain, but it may not be the most critical finding to report in this situation.
The client has epistaxis after blowing his nose several times. : Epistaxis, or a nosebleed, can occur due to high blood pressure, but it is not the most urgent or critical symptom in a hypertensive emergency. While it is essential to address the nosebleed and monitor blood pressure, other symptoms may indicate more severe consequences of uncontrolled high blood pressure.
The client has a urine output of 120 mL over 4 hours.: While decreased urine output can be a concerning sign, it is not the most significant finding to report in a hypertensive emergency. In this scenario, the focus is on acute complications related to high blood pressure, such as organ damage or impending stroke, which require immediate attention.
In summary, the finding that is most important to report to the healthcare provider in a client with a hypertensive emergency is the presence of new-onset blurry vision and facial asymmetry. These symptoms suggest potential neurological involvement and the need for urgent medical intervention to prevent serious complications like stroke.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
