A nurse is assessing a client with intermittent claudication. What client statement supports this information?
"My feet feel like I have pins and needles."
"When I stand or sit too long, my feet swell."
"My legs get a painful cramp when I walk over 30 minutes."
"I get short of breath when I climb a lot of stairs.”
The Correct Answer is C
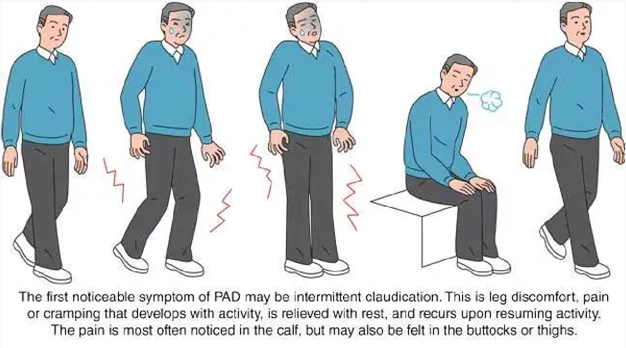
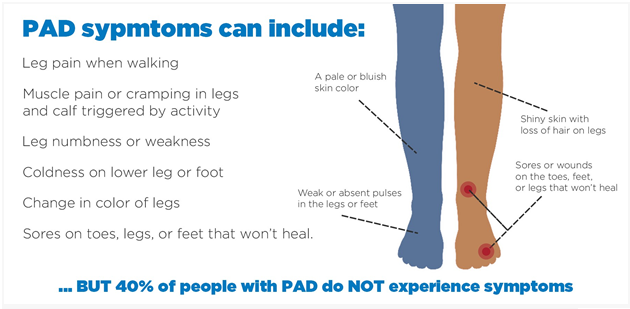
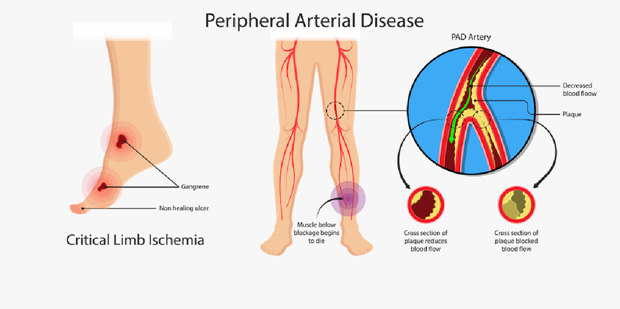
The client statement that supports the information of intermittent claudication is: "My legs get a painful cramp when I walk over 30 minutes.": Intermittent claudication is a symptom of peripheral artery disease (PAD) characterized by pain, cramping, or fatigue in the muscles of the lower extremities, typically the calves, thighs, or buttocks. This pain is usually triggered by physical activity, such as walking, and is relieved with rest. The pain is caused by inadequate blood flow and oxygen supply to the muscles due to narrowed or blocked arteries.
The other client statements do not specifically indicate intermittent claudication:
"My feet feel like I have pins and needles": This sensation of pins and needles is often associated with peripheral neuropathy, which is a condition involving nerve damage and does not directly relate to intermittent claudication.
"When I stand or sit too long, my feet swell": This statement suggests the possibility of venous insufficiency rather than intermittent claudication. Venous insufficiency involves impaired blood return from the legs to the heart and may result in swelling, aching, or heaviness in the legs.
"I get short of breath when I climb a lot of stairs": This symptom is more indicative of cardiovascular or respiratory issues, such as heart or lung disease, rather than intermittent claudication. It suggests that the client may experience exercise intolerance due to cardiopulmonary limitations.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Wear fitted closed toe shoes daily: It is important for clients with peripheral arterial disease to wear properly fitted closed toe shoes. This helps protect the feet from injury and provides support. Closed toe shoes also help maintain warmth and prevent heat loss, which is especially important for individuals with impaired circulation.
Let's review the other options and explain why they may not be appropriate:
Soak feet in warm water for an hour each day: Soaking the feet in warm water for a prolonged period can actually worsen symptoms in individuals with peripheral arterial disease. It can cause further dilation of blood vessels, leading to increased blood pooling and potential tissue damage. Therefore, soaking the feet for extended periods of time is not recommended.
Set heating pads on a low temperature: Using heating pads, especially at high temperatures, can be harmful to individuals with peripheral arterial disease. It can increase the risk of burns or thermal injury due to reduced sensation in the affected areas. Heating pads should be used with caution and on a low temperature setting, if necessary.
Use callus remover for corns or calluses: Individuals with peripheral arterial disease have reduced blood flow to the lower extremities, which can impair wound healing. It is important to avoid self-treatment of corns or calluses, as it can increase the risk of skin breakdown and infection. Clients should be advised to consult a healthcare professional, such as a podiatrist, for appropriate management of corns and calluses.
Correct Answer is C
Explanation
"I will use a heating pad on my feet at night to increase the circulation.": Using a heating pad on the feet at night is not recommended for clients with peripheral artery disease. The application of heat, such as from a heating pad, can dilate blood vessels and potentially worsen the symptoms of peripheral artery disease. This can lead to reduced blood flow to the affected limbs and increase the risk of complications.
The other client statements demonstrate an understanding of peripheral artery disease management:
"I will avoid long periods of sitting down with my legs crossed over." This statement shows awareness of the importance of maintaining good blood flow and avoiding positions that can restrict circulation.
"I will walk to the point of pain, rest, and walk again for at least 30 minutes." This statement indicates an understanding of the concept of intermittent claudication, a common symptom of peripheral artery disease. Walking until pain occurs, resting, and then resuming walking helps improve circulation and increases walking distance over time.
"I will buy some loose clothes that do not bind across my legs or waist." This statement reflects an awareness of the need to wear loose-fitting clothes that do not constrict blood flow to the legs or waist area.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
