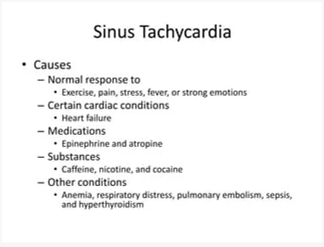
The nurse is assessing a client with a heart rate of 124 bpm. What clinical finding(s) should the nurse assess as causes of tachycardia? Select all that apply.
Blood glucose 90 mg/dL
Pain level of 10 out of 10
Temperature 101.9 F
Hemoglobin: 7g/dl
Cocaine abuse
Correct Answer : B,C,D,E
Pain level of 10 out of 10: Severe pain can stimulate the sympathetic nervous system and result in an increased heart rate.
Temperature 101.9°F: Fever can lead to an elevated heart rate as the body's response to infection or inflammation.
Hemoglobin: 7 g/dL: Low hemoglobin levels, known as anemia, can cause the heart to pump faster in an attempt to compensate for the decreased oxygen-carrying capacity of the blood.
Cocaine abuse: Cocaine is a stimulant drug that can significantly increase heart rate and cause tachycardia.
The following clinical finding would not typically be associated with tachycardia:
Blood glucose 90 mg/dL: While low or high blood glucose levels can cause symptoms, they are not directly associated with tachycardia unless they lead to significant physiological stress or hormonal imbalances.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
The most important finding to report to the health care provider would be the serum potassium level of 3.0 mEq. This is an extremely low potassium level (normal range is typically 3.5-5.0 mEq/L), which can indicate a potentially life-threatening condition called hypokalemia. Furosemide (Lasix) is a diuretic medication that can cause potassium loss in the urine, and a low potassium level can lead to serious cardiac and muscle abnormalities. It is crucial to report this finding promptly to the health care provider for appropriate intervention and monitoring.
Blood glucose level of 175 mg/dL: While an elevated blood glucose level can be a concern, especially for individuals with diabetes, it is not the most critical finding in this situation. The client's primary concern is hypertension, and the administration of IV furosemide is aimed at managing blood pressure. The elevated blood glucose level should still be addressed and monitored, but it is not as urgent as the low potassium level.
Orthostatic systolic BP decrease of 12 mm Hg: Orthostatic hypotension refers to a significant decrease in blood pressure upon standing up. While it is important to assess and manage orthostatic changes, a decrease of 12 mm Hg in systolic blood pressure alone may not be considered clinically significant. It could be a normal response for some individuals. However, if the client experiences symptoms such as dizziness or lightheadedness upon standing, further evaluation may be necessary. Nonetheless, it is not as urgent as the low potassium level.
Current blood pressure reading of 166/94 mm Hg: While this blood pressure reading indicates hypertension, it is not the most critical finding to report in this situation. The nurse is preparing to administer furosemide (Lasix), which is a medication commonly used to treat hypertension. It is expected that the blood pressure will be high before administering the medication. The goal is to monitor the blood pressure after the administration to assess the effectiveness of the medication.
Correct Answer is B
Explanation
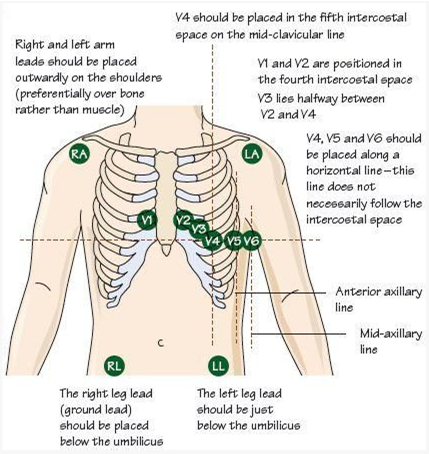
The most appropriate nursing intervention to improve adhesion of the ECG leads on a male client with abundant chest hair is to clip the chest hair with the patient's permission before applying the leads. Chest hair can interfere with the adhesion of the ECG leads, resulting in poor signal quality and potentially affecting the accuracy of the ECG recording. By clipping the chest hair, the nurse can improve the contact between the skin and the ECG leads, allowing for better adhesion and signal transmission.
It is important to obtain the patient's permission before clipping the chest hair to respect their autonomy and ensure their comfort during the procedure. The nurse should explain the reason for clipping the hair and address any concerns or questions the patient may have.
Let's review the other options and explain why they are not the most appropriate interventions:
Using alcohol swabs to clean the skin before applying the leads: While cleaning the skin with alcohol swabs is a routine practice to remove oils and dirt that can affect adhesion, it may not be sufficient in the presence of abundant chest hair. Clipping the hair would be more effective in this situation.
Applying the leads to the arms and legs only: This option would not provide an accurate 12-lead ECG recording, as the chest leads are essential for evaluating the electrical activity of the heart from different angles. It is important to have the leads properly placed on the chest for an accurate assessment.
Rescheduling the ECG: Unless there are other valid reasons for rescheduling, such as a medical condition that contraindicates the procedure, rescheduling solely due to abundant chest hair would be unnecessary. Clipping the hair is a practical and effective solution to improve adhesion.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
