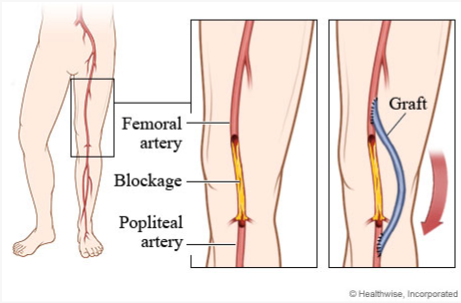
A client who has undergone a femoral to popliteal bypass graft surgery returns to the surgical unit. Which assessments should the nurse perform during the first postoperative day?
Assess pulse of affected extremity every 15 minutes at first.
Palpate the affected leg for pain during every assessment
Assess the client for signs and symptoms of compartment syndrome every 2 hours.
Perform Doppler evaluation once daily.
Correct Answer : A,B,C,D
Assess pulse of the affected extremity every 15 minutes at first: Frequent assessment of the pulse in the affected extremity is important to monitor for any changes in blood flow. This allows the nurse to identify any potential complications such as graft occlusion or compromised circulation promptly.
Palpate the affected leg for pain during every assessment: Assessing for pain in the affected leg is crucial to identify any signs of ischemia or inadequate perfusion. Increased pain could indicate reduced blood flow or other complications that require immediate attention.
Assess the client for signs and symptoms of compartment syndrome every 2 hours: Compartment syndrome can occur after vascular surgeries, and early recognition is vital. The nurse should assess for signs and symptoms such as pain, numbness, tingling, increased swelling, and tense compartments. Regular assessment every 2 hours can help detect compartment syndrome promptly and prevent further complications.
Perform Doppler evaluation once daily: Doppler evaluation may be ordered by the healthcare provider to assess blood flow and graft patency. However, the frequency of Doppler evaluation may vary depending on the client's condition and the healthcare provider's orders. Once daily assessment is not sufficient if there are concerns regarding blood flow or graft viability.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
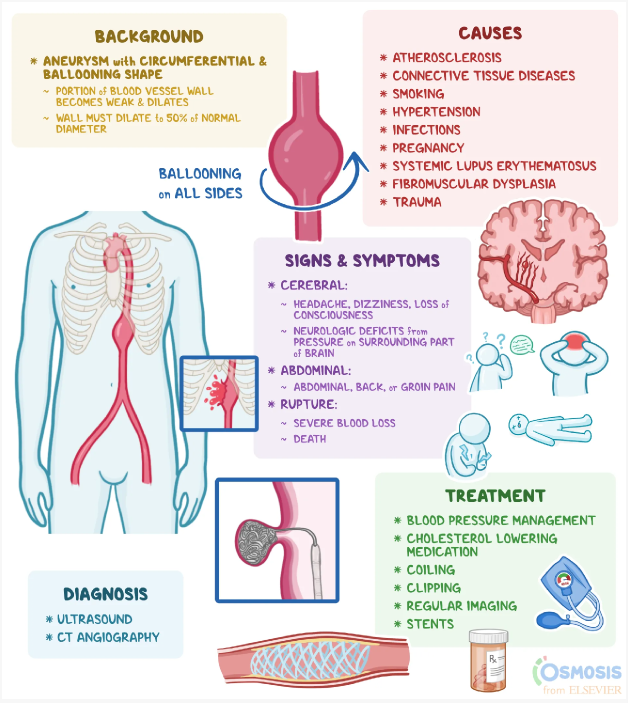
Correct Answer is B
Explanation
Abdominal aortic aneurysms (AAA) often do not present with specific symptoms in the early stages. It is not uncommon for individuals with AAA to be asymptomatic or have vague symptoms. Therefore, the absence of abdominal pain or any problems related to the abdomen is a common finding during the assessment of a client with an abdominal aortic aneurysm.
Let's briefly review the other statements:
"I have stomach pain every time I eat a big, heavy meal": This statement is more suggestive of gastrointestinal issues such as indigestion or acid reflux rather than specifically related to an abdominal aortic aneurysm.
"I have periodic episodes of constipation and then diarrhea": This statement may indicate gastrointestinal issues, but it is not a typical symptom associated with an abdominal aortic aneurysm. AAA is primarily related to the aorta, the main blood vessel in the abdomen, and its symptoms are not directly linked to bowel function.
"I belch a lot, especially when I lay down after eating": This statement suggests gastrointestinal symptoms such as acid reflux or gastroesophageal reflux disease (GERD). While these symptoms may be unrelated to the abdominal aortic aneurysm itself, they can coexist with other conditions.
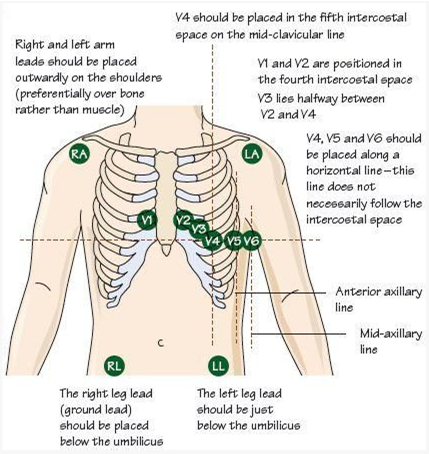
Correct Answer is B
Explanation
The most appropriate nursing intervention to improve adhesion of the ECG leads on a male client with abundant chest hair is to clip the chest hair with the patient's permission before applying the leads. Chest hair can interfere with the adhesion of the ECG leads, resulting in poor signal quality and potentially affecting the accuracy of the ECG recording. By clipping the chest hair, the nurse can improve the contact between the skin and the ECG leads, allowing for better adhesion and signal transmission.
It is important to obtain the patient's permission before clipping the chest hair to respect their autonomy and ensure their comfort during the procedure. The nurse should explain the reason for clipping the hair and address any concerns or questions the patient may have.
Let's review the other options and explain why they are not the most appropriate interventions:
Using alcohol swabs to clean the skin before applying the leads: While cleaning the skin with alcohol swabs is a routine practice to remove oils and dirt that can affect adhesion, it may not be sufficient in the presence of abundant chest hair. Clipping the hair would be more effective in this situation.
Applying the leads to the arms and legs only: This option would not provide an accurate 12-lead ECG recording, as the chest leads are essential for evaluating the electrical activity of the heart from different angles. It is important to have the leads properly placed on the chest for an accurate assessment.
Rescheduling the ECG: Unless there are other valid reasons for rescheduling, such as a medical condition that contraindicates the procedure, rescheduling solely due to abundant chest hair would be unnecessary. Clipping the hair is a practical and effective solution to improve adhesion.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
