The nurse is providing discharge education to a client with hypertension. Which essential information should the nurse include in the teaching plan?
Maintaining a low-potassium diet
Skipping a medication dose if dizziness occurs
Maintaining a 2 gram-sodium diet
Drink three glasses of wine a day
The Correct Answer is C
Maintaining a 2 gram-sodium (salt) diet is an important aspect of managing hypertension. High sodium intake can contribute to elevated blood pressure. Therefore, reducing sodium intake is recommended to help control blood pressure levels. The nurse should provide guidance on reading food labels, avoiding high-sodium processed foods, and incorporating a diet rich in fruits, vegetables, and whole grains.
The other options listed are not appropriate or beneficial for managing hypertension:
Maintaining a low-potassium diet: Potassium is an essential mineral that helps regulate blood pressure. While specific potassium restrictions may be necessary for some individuals with certain medical conditions, most people with hypertension do not need to limit their potassium intake. In fact, a balanced diet with adequate potassium is generally recommended.
Skipping a medication dose if dizziness occurs: It is not advisable to skip medication doses without consulting a healthcare provider. Hypertension medications are prescribed to help control blood pressure, and missing doses can lead to uncontrolled hypertension and potential complications. If the client experiences dizziness or other side effects from the medication, they should consult their healthcare provider for appropriate management.
Drinking three glasses of wine a day: Excessive alcohol consumption can contribute to elevated blood pressure. The recommended alcohol intake for individuals with hypertension is moderate or limited to moderate levels, which typically means no more than one drink per day for women and two drinks per day for men. Drinking excessive amounts of wine or any alcoholic beverage can negatively affect blood pressure control.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
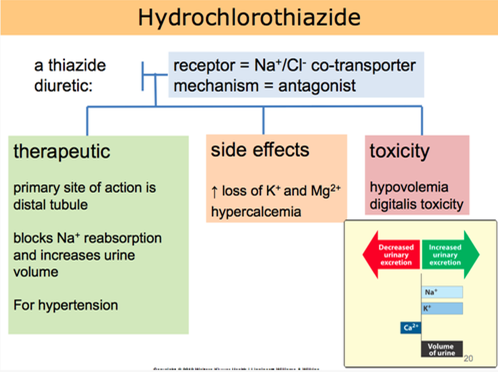
Hydrochlorothiazide is a diuretic medication commonly prescribed for hypertension. It works by increasing urine output, which helps to reduce fluid volume and lower blood pressure. Taking the medication in the morning is beneficial because the increased urine production during the day can help prevent nighttime disruptions due to frequent urination.
Let's go through the other statements and explain why they are not accurate:
"I will not take this medicine when my blood pressure is okay":
This statement indicates a misunderstanding about the purpose of hydrochlorothiazide. It is important to take prescribed medications consistently, even when blood pressure readings are within the normal range, as they are intended to help maintain blood pressure control.
"I will check blood pressure in both arms and legs before taking the drug":
Checking blood pressure in both arms and legs is not directly related to hydrochlorothiazide use. Blood pressure should be monitored regularly, but it is not necessary to perform these measurements specifically before taking the medication.
"I will decrease potassium foods such as bananas in my diet":
Hydrochlorothiazide can cause potassium loss as a side effect. However, reducing potassium-rich foods without healthcare provider guidance may not be appropriate. It is important for the client to discuss dietary adjustments and potassium supplementation with their healthcare provider if needed.
Correct Answer is A
Explanation
Hypertension is typically diagnosed when a person's blood pressure consistently exceeds 130/80 mm Hg on multiple occasions. However, the specific target blood pressure for treatment may vary based on individual factors and the presence of other comorbidities.
Among the options provided, a blood pressure reading of 128/76 mm Hg is within the target range for many individuals with hypertension. The systolic pressure (128 mm Hg) is below the threshold of 130 mm Hg, and the diastolic pressure (76 mm Hg) is below the threshold of 80 mm Hg.
The other blood pressure readings would warrant further evaluation or possible changes in therapy:
128/92 mm Hg: The diastolic pressure (92 mm Hg) is above the threshold of 80 mm Hg, indicating uncontrolled hypertension.
98/56 mm Hg: This blood pressure reading is below the threshold for hypertension, but it is considered low and may require further assessment to determine if it is normal for the individual or if it indicates hypotension.
142/78 mm Hg: While the systolic pressure (142 mm Hg) is slightly above the threshold of 130 mm Hg, it may not necessarily require immediate changes in therapy. However, it should be closely monitored to ensure blood pressure control.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
