The client is diagnosed with an abdominal aortic aneurysm. Which statement would the nurse expect the client to make during the admission assessment?
“I have stomach pain every time I eat a big, heavy meal."
“I don't have any abdominal pain or any type of problems."
“I have periodic episodes of constipation and then diarrhea."
“I belch a lot especially when I lay down after eating"
The Correct Answer is B
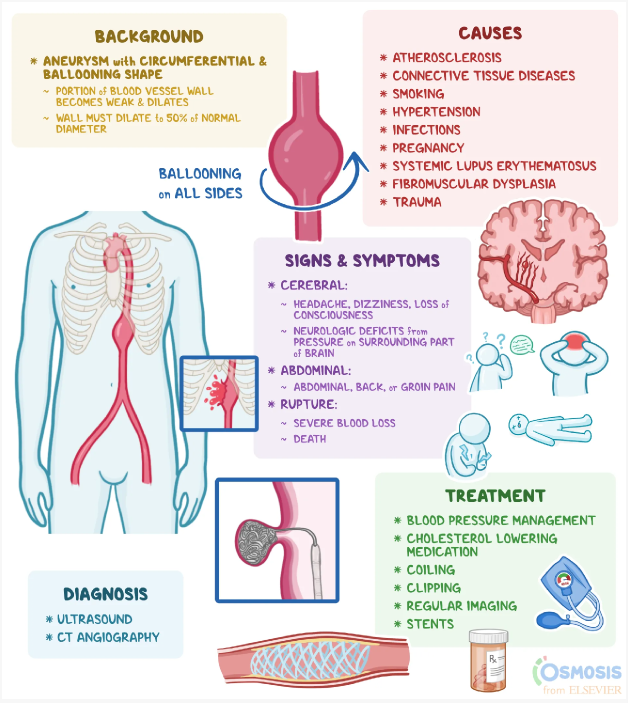
Abdominal aortic aneurysms (AAA) often do not present with specific symptoms in the early stages. It is not uncommon for individuals with AAA to be asymptomatic or have vague symptoms. Therefore, the absence of abdominal pain or any problems related to the abdomen is a common finding during the assessment of a client with an abdominal aortic aneurysm.
Let's briefly review the other statements:
"I have stomach pain every time I eat a big, heavy meal": This statement is more suggestive of gastrointestinal issues such as indigestion or acid reflux rather than specifically related to an abdominal aortic aneurysm.
"I have periodic episodes of constipation and then diarrhea": This statement may indicate gastrointestinal issues, but it is not a typical symptom associated with an abdominal aortic aneurysm. AAA is primarily related to the aorta, the main blood vessel in the abdomen, and its symptoms are not directly linked to bowel function.
"I belch a lot, especially when I lay down after eating": This statement suggests gastrointestinal symptoms such as acid reflux or gastroesophageal reflux disease (GERD). While these symptoms may be unrelated to the abdominal aortic aneurysm itself, they can coexist with other conditions.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["D","E"]
Explanation
The traces that should require immediate follow-up by the nurse are:
● Pacer spikes occur directly before the T waves.
Pacer spikes occurring on the T waves indicate an issue with the pacemaker's timing or sensing. This could lead to inappropriate pacing or pacing during the refractory period, which can be detrimental to the client's heart function.
● The heart rate is outside of programmed parameters.
If the heart rate is outside of the programmed parameters set for the client's pacemaker, it may indicate a malfunction or failure of the device or a change in the client's cardiac status. It is important for the nurse to assess the client's condition and notify the healthcare provider for further evaluation and intervention.
Let's review the other options and explain why they do not require immediate follow-up:
Pacer spikes are adequate in number: This indicates that the pacemaker is delivering the appropriate number of electrical impulses as programmed. As long as the other parameters are normal, this finding does not require immediate follow-up.
Pacer spikes occur directly before the P waves: This is the desired and expected pattern for a pacemaker in normal sinus rhythm. It indicates proper timing and coordination between the pacemaker and the client's intrinsic electrical activity.
Pacer spikes occur directly before the QRS waves: This is also the desired and expected pattern for a pacemaker in clients with ventricular pacing. It indicates proper timing and coordination between the pacemaker and the client's intrinsic electrical activity.
The heart rate is within programmed parameters: If the heart rate falls within the programmed parameters set for the client's pacemaker, it indicates that the device is functioning appropriately in maintaining the desired heart rate.
Correct Answer is D
Explanation
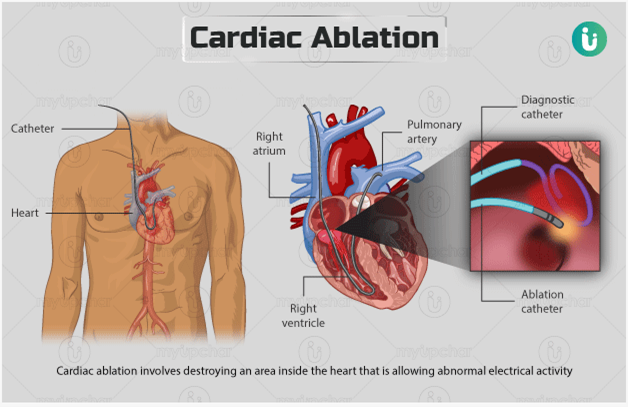
The procedure uses electrical energy to destroy areas of the conduction system: Catheter ablation is a minimally invasive procedure performed to treat abnormal heart rhythms, such as atrial flutter. During the procedure, a catheter is inserted into the heartand used to deliver electrical energy to specific areas of the heart tissue. This energy is used to destroy or ablate the abnormal conduction pathways that are causing the atrial flutter.
Let's go through the other options and explain why they are not accurate:
The procedure stimulates the growth of new pathways between the atria: Catheter ablation does not stimulate the growth of new pathways. Instead, it aims to eliminate or modify existing abnormal pathways in the heart to restore normal electrical conduction.
The procedure uses cold therapy to stop the formation of the flutter waves: Catheter ablation does not use cold therapy. It primarily utilizes radiofrequency energy or other sources of heat to ablate the targeted areas of the heart tissue.
The procedure prevents or minimizes the patient's risk for sudden cardiac death: While catheter ablation can be an effective treatment for certain arrhythmias, including atrial flutter, it is not primarily performed to prevent or minimize the risk of sudden cardiac death. Its main purpose is to restore normal heart rhythm and alleviate symptoms associated with the arrhythmia.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
