The nurse is obtaining a systolic blood pressure by palpation. While inflating the cuff, the radial pulse is no longer palpable at 90 mm Hg. Which action should the nurse take?
Document the absence of the radial pulse.
Release the manometer valve immediately.
Inflate blood pressure cuff to 120 mm Hg.
Record a palpable systolic pressure of 90 mm Hg.
The Correct Answer is C
A. Document the absence of the radial pulse:
While it's important to document findings accurately, it's also crucial to ensure that blood pressure measurements are obtained correctly. If the radial pulse becomes unpalpable before reaching the expected systolic pressure, further action is needed to obtain an accurate measurement.
B. Release the manometer valve immediately:
Releasing the manometer valve immediately would lead to deflating the cuff and potentially missing the opportunity to obtain an accurate blood pressure measurement. This action is not appropriate at this stage.
C. Inflate blood pressure cuff to 120 mm Hg:
When the radial pulse becomes unpalpable during cuff inflation, it indicates that the cuff pressure is above the systolic pressure. To accurately determine the systolic pressure, the cuff should be inflated to a higher pressure (usually 20-30 mm Hg above the point where the radial pulse disappears) and then slowly deflated while palpating for the return of the radial pulse.
D. Record a palpable systolic pressure of 90 mm Hg:
If the radial pulse is no longer palpable at 90 mm Hg, this suggests that the true systolic pressure is higher than 90 mm Hg. Recording a palpable systolic pressure of 90 mm Hg without further action would likely underestimate the true systolic pressure.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
A. Document the absence of the radial pulse:
While it's important to document findings accurately, it's also crucial to ensure that blood pressure measurements are obtained correctly. If the radial pulse becomes unpalpable before reaching the expected systolic pressure, further action is needed to obtain an accurate measurement.
B. Release the manometer valve immediately:
Releasing the manometer valve immediately would lead to deflating the cuff and potentially missing the opportunity to obtain an accurate blood pressure measurement. This action is not appropriate at this stage.
C. Inflate blood pressure cuff to 120 mm Hg:
When the radial pulse becomes unpalpable during cuff inflation, it indicates that the cuff pressure is above the systolic pressure. To accurately determine the systolic pressure, the cuff should be inflated to a higher pressure (usually 20-30 mm Hg above the point where the radial pulse disappears) and then slowly deflated while palpating for the return of the radial pulse.
D. Record a palpable systolic pressure of 90 mm Hg:
If the radial pulse is no longer palpable at 90 mm Hg, this suggests that the true systolic pressure is higher than 90 mm Hg. Recording a palpable systolic pressure of 90 mm Hg without further action would likely underestimate the true systolic pressure.
Correct Answer is A
Explanation
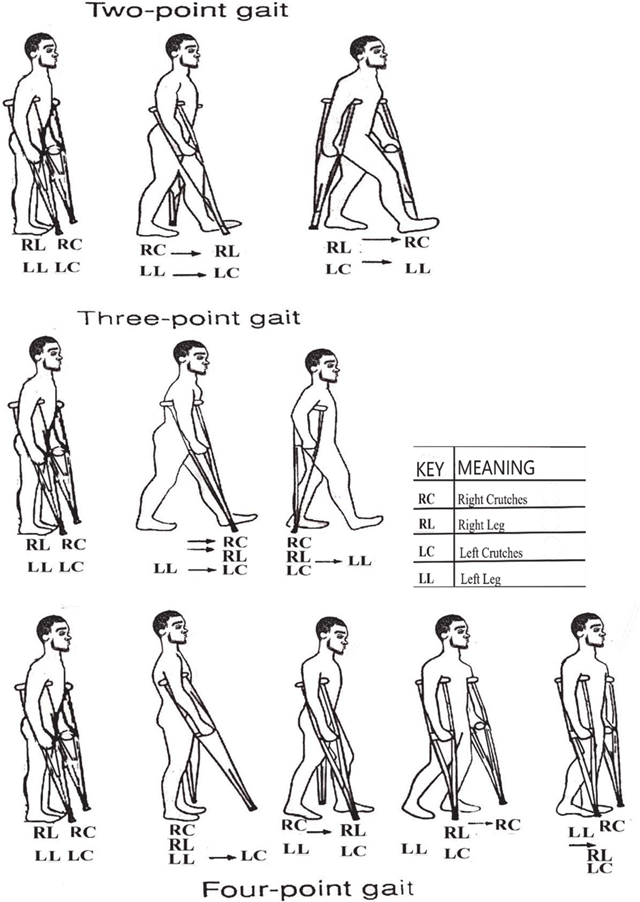
A. Progresses to foot touchdown and weight bearing of affected leg:
This choice indicates that the client understands proper crutch walking because it involves the correct progression of weight-bearing on the affected leg while using the crutches for support. In the three-point gait crutch walking technique, the client progresses by first touching down the foot of the affected leg and then transferring weight onto that leg while stepping forward with the crutches. This behavior ensures proper balance and support during ambulation.
B. Practices bicep and triceps isometric exercises:
This choice does not directly indicate understanding of proper crutch walking. While strengthening the biceps and triceps muscles can be beneficial for overall strength and endurance, it is not a specific behavior related to proper crutch walking technique.
C. Inspects crutches to ensure rubber tips are intact:
While it is important to inspect crutches regularly to ensure they are in good condition, this behavior alone does not necessarily indicate an understanding of proper crutch walking technique. It is more related to equipment maintenance and safety rather than the actual execution of crutch walking.
D. Bears body weight on the palms of hands during the crutch gait:
This choice suggests an incorrect technique. Proper crutch walking technique involves bearing weight on the hands through the hand grips of the crutches rather than the palms. Placing excessive weight on the palms can lead to discomfort, injury, and improper weight distribution, which could hinder effective ambulation.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
