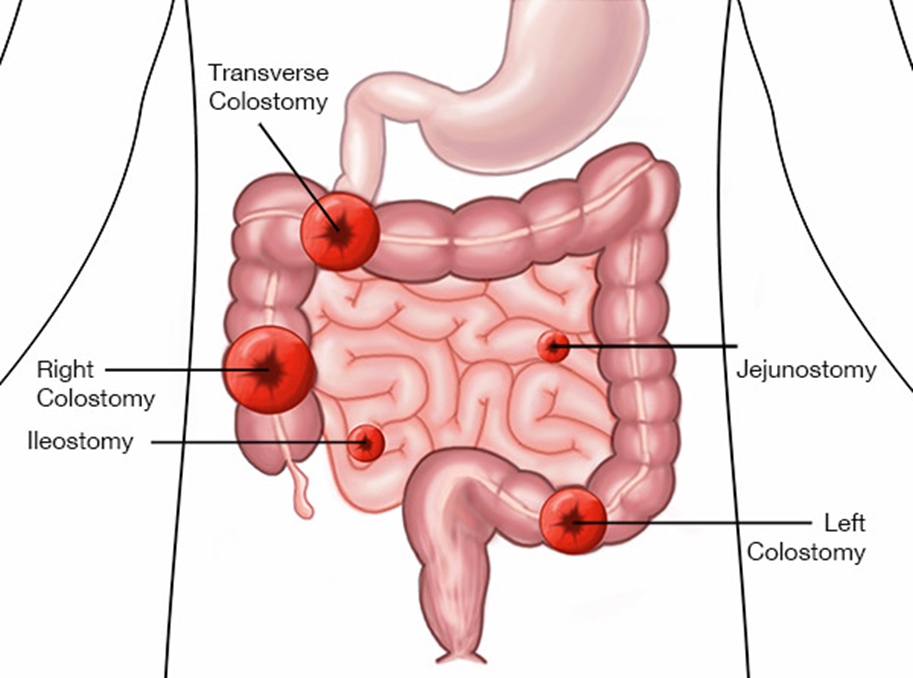
The nurse is caring for a client with an ileostomy because of inflammatory bowel disease. Which assessment findings indicate to the nurse that the ileostomy is functioning as expected? Select all that apply.
Formed stool in collection pouch.
Stoma is edematous and bleeding.
Stoma is pink and shiny.
Skin excoriation around the stoma.
Mucus liquid flows from the stoma.
Correct Answer : C,E
Choice A: Formed stool in collection pouch
Formed stool in the collection pouch is not expected in an ileostomy. The output from an ileostomy is typically liquid to semi-liquid because the ileum does not absorb as much water as the colon. If formed stool is present, it may indicate a blockage or other issue that needs to be addressed.
Choice B: Stoma is edematous and bleeding
An edematous and bleeding stoma is not a normal finding and may indicate complications such as infection, trauma, or poor stoma care. The stoma should be moist and pink, but not swollen or bleeding. Persistent bleeding or significant edema should be reported to a healthcare provider immediately.
Choice C: Stoma is pink and shiny
A pink and shiny stoma is a sign that the ileostomy is functioning well. This indicates good blood flow and healthy tissue. The stoma should always appear moist and pink, similar to the inside of the mouth. Any deviation from this appearance, such as a pale, dark, or dry stoma, should be evaluated by a healthcare professional.
Choice D: Skin excoriation around the stoma
Skin excoriation around the stoma is not a normal finding and suggests that the skin is being irritated by the stoma output or the ostomy appliance. Proper skin care and fitting of the ostomy appliance are essential to prevent skin breakdown. If excoriation occurs, it should be treated promptly to prevent further complications.
Choice E: Mucus liquid flows from the stoma
Mucus liquid flowing from the stoma is expected in an ileostomy. The output is typically liquid to semi-liquid and may contain mucus, which is normal for the small intestine. This type of output indicates that the ileostomy is functioning as intended.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A reason:
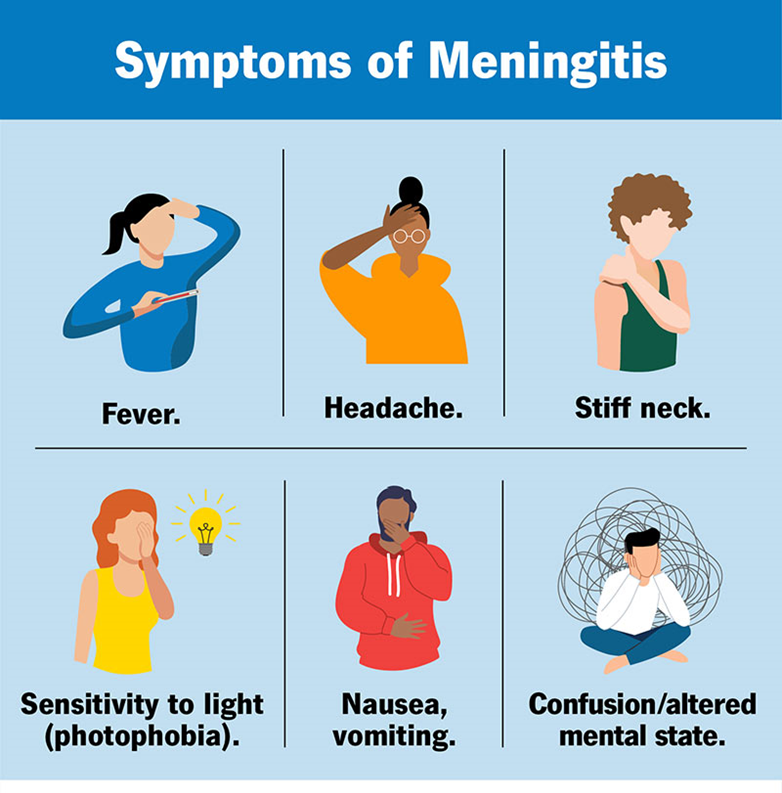
Strict monitoring of hourly intake and output is important for managing fluid balance and detecting potential complications such as dehydration or fluid overload1. However, it is not the highest priority in the acute phase of bacterial meningitis. The primary concern is to monitor for signs of increased intracranial pressure (ICP) and neurological deterioration.
Choice B reason:
Managing pain through drug and non-drug methods is essential for patient comfort and overall well-being. Pain management can help reduce stress and improve the patient’s ability to rest and recover. However, it is not the highest priority compared to monitoring neurological status, which can provide early indications of complications such as increased ICP or seizures.
Choice C reason:
Assessing neurological status at least every 2 to 4 hours is the highest priority for a client with bacterial meningitis. This frequent assessment helps detect early signs of neurological deterioration, increased ICP, and other complications. Early detection and intervention are crucial in preventing severe outcomes and improving the patient’s prognosis.
Choice D reason:
Decreasing environmental stimuli is important to reduce stress and prevent exacerbation of symptoms such as headache and photophobia. While this intervention is beneficial, it is not as critical as frequent neurological assessments in the acute management of bacterial meningitis.
Correct Answer is ["A"]
Explanation
Choice A Reason:
Suction equipment at the bedside.
Having suction equipment at the bedside is crucial for a client with status epilepticus. During a seizure, there is a risk of aspiration due to excessive salivation or vomiting. Suction equipment allows the nurse to quickly clear the airway, preventing aspiration and ensuring the client can breathe properly. This precaution is essential to maintain the client’s airway and prevent complications such as aspiration pneumonia.
Choice B Reason:
Continuous sedation.
Continuous sedation is not typically a standard precaution for all clients with status epilepticus. While sedation may be necessary in some cases to control seizures, it is not a universal precaution. The primary goal is to stop the seizure activity and stabilize the client. Continuous sedation may be used in specific situations under close medical supervision, but it is not a general precaution that nurses implement for all clients with status epilepticus.
Choice C Reason:
Side rails padded.
Padding the side rails of the bed is an important precaution to prevent injury during a seizure. Clients experiencing seizures may have uncontrolled movements, which can lead to injury if they hit the hard surfaces of the bed. Padded side rails help to cushion these impacts, reducing the risk of bruises, cuts, or fractures. This precaution is essential for ensuring the client’s safety during seizure activity.
Choice D Reason:
Bed in low position.
Keeping the bed in a low position is another important safety measure. If a client with status epilepticus were to fall out of bed during a seizure, the lower height reduces the risk of serious injury. This precaution helps to minimize the impact of any potential falls, ensuring the client’s safety. It is a simple yet effective measure to prevent harm during seizure episodes.
Choice E Reason:
Intravenous (IV) access.
Establishing intravenous (IV) access is critical for a client with status epilepticus. IV access allows for the rapid administration of medications needed to control seizures and manage the client’s condition. In an emergency, quick access to the bloodstream is essential for delivering life-saving treatments. This precaution ensures that the medical team can promptly and effectively intervene to stop the seizure activity.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
