An acute care nurse receives a shift report for a client who has increased intracranial pressure. The nurse is told that the client demonstrates decorticate posturing. Which of the following findings should the nurse expect to observe when assessing the client?
Pronation of the hands.
Extension of the arms.
External rotation of the lower extremities.
Plantar flexion of the legs.
The Correct Answer is D
Choice A Reason:
Pronation of the hands.
Pronation of the hands is not typically associated with decorticate posturing. Decorticate posturing is characterized by the flexion of the arms and wrists, with the hands often clenched into fists. Pronation refers to the rotation of the hands so that the palms face downward, which is not a feature of decorticate posturing.
Choice B Reason:
Extension of the arms.
Extension of the arms is more characteristic of decerebrate posturing, not decorticate posturing. In decorticate posturing, the arms are flexed and held tightly to the chest, not extended. This flexion is due to damage to the cerebral hemispheres, which affects the corticospinal tract.
Choice C Reason:
External rotation of the lower extremities.
External rotation of the lower extremities is not a typical finding in decorticate posturing. In decorticate posturing, the legs are usually extended and rigid, with the toes pointed. External rotation would indicate a different type of posturing or neurological condition.
Choice D Reason:
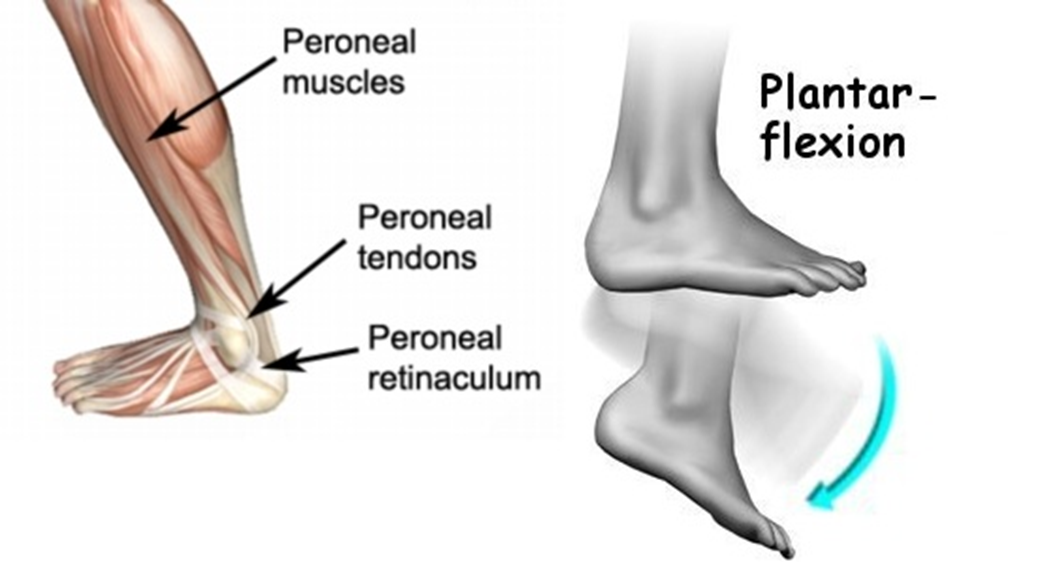
Plantar flexion of the legs.
Plantar flexion of the legs is a characteristic finding in decorticate posturing. This involves the toes pointing downward, which is a result of the increased muscle tone and reflexes due to the brain injury. This posture indicates severe damage to the brain, specifically the corticospinal tract.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A Reason:
Weigh the client daily: While monitoring weight is important for clients with Addison’s disease, it is not the primary action to prevent an Addisonian crisis. Daily weight monitoring helps track fluid balance and detect any sudden changes that might indicate complications, but it does not directly address the hormonal imbalance that characterizes Addisonian crisis.
Choice B Reason:
Restrict food intake: Restricting food intake is not recommended for clients with Addison’s disease. Proper nutrition is crucial for maintaining energy levels and overall health. Clients with Addison’s disease need a balanced diet to manage their condition effectively. Restricting food intake could lead to malnutrition and exacerbate symptoms.
Choice C Reason:
Administer oral corticosteroids: This is the correct action. Addison’s disease is characterized by insufficient production of cortisol and aldosterone by the adrenal glands. Administering oral corticosteroids helps replace the deficient hormones and manage the symptoms of Addison’s disease. During an Addisonian crisis, immediate administration of corticosteroids is critical to prevent severe complications such as shock, coma, or even death.
Choice D Reason:
Provide a low carbohydrate diet: A low carbohydrate diet is not specifically recommended for clients with Addison’s disease. Instead, a balanced diet that includes adequate carbohydrates, proteins, and fats is essential. Carbohydrates are important for maintaining energy levels, especially since clients with Addison’s disease may experience fatigue and weakness. Restricting carbohydrates could lead to low blood sugar levels, which can be dangerous for these clients.
Correct Answer is ["A","B","C","D"]
Explanation
Choice A reason: A buffalo hump is a characteristic sign of Cushing’s syndrome. It refers to the accumulation of fat on the back of the neck and shoulders. This symptom occurs due to the excessive production of cortisol, which leads to abnormal fat distribution in the body.
Choice B reason: Moon face is another hallmark of Cushing’s syndrome. It describes the rounding and fullness of the face, which results from fat deposits. This symptom is also caused by prolonged exposure to high levels of cortisol.
Choice C reason: Hypertension, or high blood pressure, is commonly associated with Cushing’s syndrome. Cortisol increases blood pressure by enhancing the sensitivity of blood vessels to catecholamines and by promoting sodium and water retention.
Choice D reason: Purple striations, or stretch marks, are often seen in individuals with Cushing’s syndrome. These marks typically appear on the abdomen, thighs, breasts, and arms. They result from the thinning of the skin and the breakdown of collagen due to elevated cortisol levels.
Choice E reason: Tremors are not typically associated with Cushing’s syndrome. While Cushing’s syndrome can cause a variety of symptoms, tremors are more commonly linked to other conditions such as hyperthyroidism or neurological disorders.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
