A nurse suspects a client has diabetes insipidus. What are the priority interventions? Select all that apply.
Monitor for hypernatremia.
Monitor neuro status.
Monitor for hyponatremia.
Monitor urine specific gravity.
Monitor strict I&O.
Correct Answer : A
Choice A: Monitor for hypernatremia.
Hypernatremia, or high sodium levels in the blood, is a common complication of diabetes insipidus due to excessive water loss and insufficient water intake. Monitoring for hypernatremia involves regular blood tests to check sodium levels. Symptoms of hypernatremia include extreme thirst, confusion, muscle twitching, and seizures. Early detection and management are crucial to prevent severe complications.
Choice B: Monitor neuro status.
Monitoring neurological status is essential in patients with diabetes insipidus because severe hypernatremia can lead to neurological symptoms such as confusion, irritability, seizures, and even coma. Regular assessments of mental status, level of consciousness, and neurological function help in early detection of complications and timely intervention.
Choice C: Monitor for hyponatremia.
While hyponatremia (low sodium levels) is less common in diabetes insipidus, it can occur if there is excessive water intake without adequate sodium replacement. Symptoms include headache, nausea, vomiting, confusion, and seizures. Monitoring sodium levels helps in maintaining a balance and preventing complications.
Choice D: Monitor urine specific gravity.
Urine specific gravity measures the concentration of solutes in the urine. In diabetes insipidus, urine is typically very dilute, with a specific gravity of less than 1.005. Regular monitoring helps in assessing the effectiveness of treatment and the patient’s hydration status. It also aids in differentiating diabetes insipidus from other conditions with similar symptoms.
Choice E: Monitor strict I&O.
Strict monitoring of intake and output (I&O) is crucial in managing diabetes insipidus. This involves accurately measuring all fluids consumed and excreted to ensure proper hydration and electrolyte balance. It helps in identifying trends in fluid loss and guiding appropriate fluid replacement therapy.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A Reason:
Assessing the client’s gag reflex before giving any food or water is crucial after a bronchoscopy. The procedure involves the use of local anesthesia to numb the throat, which can impair the gag reflex and increase the risk of aspiration. Ensuring that the gag reflex has returned before allowing the client to eat or drink helps prevent choking and aspiration, which are serious complications.
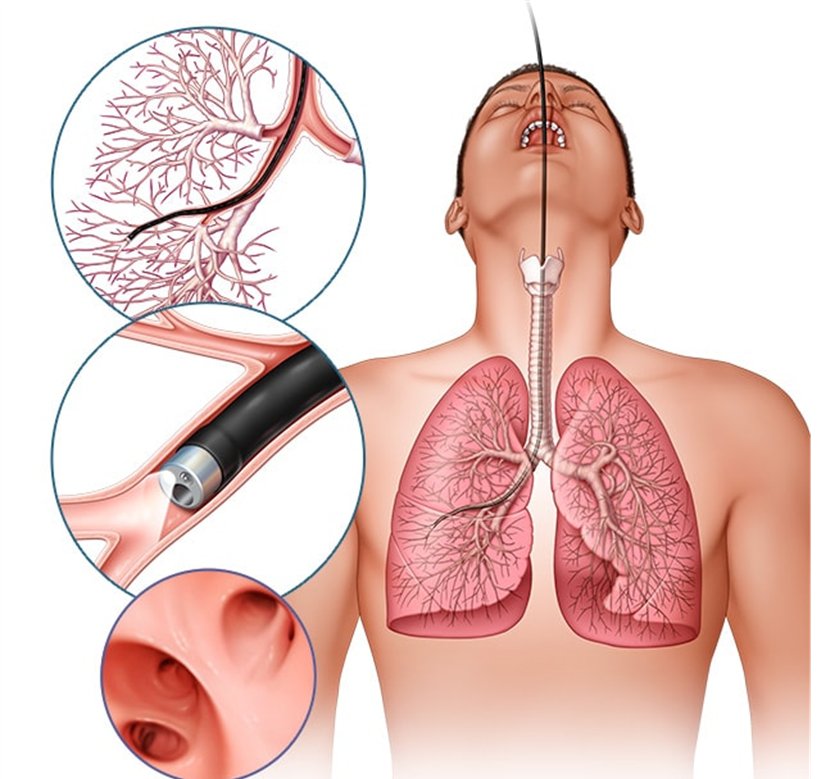
Choice B Reason:
Providing the client with ice chips instead of a drink of water is not the best initial action. While ice chips may seem like a safer option, they still pose a risk of aspiration if the gag reflex has not fully returned. The priority is to first assess the gag reflex to ensure the client can safely swallow.
Choice C Reason:
Contacting the primary healthcare provider and getting the appropriate orders is not necessary as the first action. The nurse can independently assess the gag reflex, which is a standard nursing practice after procedures involving throat anesthesia. If there are concerns after the assessment, then contacting the healthcare provider would be appropriate.
Choice D Reason:
Letting the client have a small sip to evaluate the ability to swallow is not safe without first assessing the gag reflex. This approach could lead to aspiration if the gag reflex has not returned. The initial step should always be to assess the gag reflex to ensure the client can safely swallow liquids.
Correct Answer is ["A","C","E"]
Explanation
Choice A Reason:
Weight loss.
Weight loss is a common symptom of hyperthyroidism. This condition speeds up the body’s metabolism, causing the body to burn calories more quickly than usual. Despite an increased appetite, individuals with hyperthyroidism often experience significant weight loss. This symptom is a direct result of the overproduction of thyroid hormones, which increases the metabolic rate.
Choice B Reason:
Intolerance to cold.
Intolerance to cold is not typically associated with hyperthyroidism; it is more commonly a symptom of hypothyroidism. Hyperthyroidism usually causes heat intolerance due to the increased metabolic rate, which raises the body’s temperature. Therefore, this choice is not relevant to hyperthyroidism.
Choice C Reason:
An elevated systolic blood pressure.
An elevated systolic blood pressure can be a symptom of hyperthyroidism. The increased levels of thyroid hormones can cause the heart to work harder, leading to higher blood pressure. This symptom is important to monitor as it can lead to further cardiovascular complications if left untreated.
Choice D Reason:
A heart rate of 90 bpm.
A heart rate of 90 bpm is within the normal range for adults and is not specifically indicative of hyperthyroidism. Hyperthyroidism typically causes a rapid or irregular heartbeat, often exceeding 100 bpm. Therefore, this choice does not accurately reflect a clinical manifestation of hyperthyroidism.
Choice E Reason:
Increased fatigability.
Increased fatigability is a common symptom of hyperthyroidism. Despite the increased metabolic rate, individuals with hyperthyroidism often feel tired and weak. This paradoxical symptom occurs because the body’s systems are overworked and cannot sustain the heightened activity levels, leading to fatigue.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
