A client is receiving baclofen for the management of symptoms associated with multiple sclerosis. To evaluate the effectiveness of this medication, what does the nurse assess?
Muscle spasms
Mood and affect
Appetite
Sleep pattern
The Correct Answer is A
Choice A reason:
Baclofen is primarily used to treat muscle symptoms caused by multiple sclerosis, including muscle spasms, stiffness, and pain1. It acts on the spinal cord nerves to decrease the number and severity of muscle spasms, thereby improving muscle movement2. The effectiveness of baclofen in managing multiple sclerosis symptoms is best evaluated by assessing the reduction in muscle spasms.

Choice B reason:
While mood and affect are important aspects of a patient’s overall well-being, they are not the primary indicators of baclofen’s effectiveness. Baclofen does not have a direct impact on mood and affect, as its main function is to relieve muscle spasms and improve muscle movement.
Choice C reason:
Appetite is not a primary concern when evaluating the effectiveness of baclofen. This medication is not known to significantly affect appetite. The main therapeutic goal of baclofen is to reduce muscle spasms and improve mobility in patients with multiple sclerosis.
Choice D reason:
Sleep pattern, although important for overall health, is not the primary measure of baclofen’s effectiveness. Baclofen’s primary role is to alleviate muscle spasms and improve muscle function. While it may have some impact on sleep due to its muscle-relaxing properties, this is not the main criterion for evaluating its effectiveness.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["A","B","C","D","E"]
Explanation
Choice A Reason:
Monitoring the QT interval is crucial when administering amiodarone because this drug can prolong the QT interval, increasing the risk of torsades de pointes, a potentially life-threatening type of ventricular tachycardia. Regular monitoring helps in early detection and management of this adverse effect, ensuring patient safety.
Title: Choice B Reason:
Heart rate monitoring is essential as amiodarone can cause bradycardia (slow heart rate). Continuous monitoring allows the nurse to detect any significant changes in heart rate and take appropriate actions, such as adjusting the medication dosage or providing interventions to manage bradycardia.
Title: Choice C Reason:
Respiratory rate monitoring is necessary because amiodarone can cause pulmonary toxicity, including interstitial pneumonitis and acute respiratory distress syndrome (ARDS). By keeping track of the respiratory rate, the nurse can identify early signs of respiratory complications and intervene promptly
Title: Choice D Reason:
Heart rhythm monitoring is vital since amiodarone is used to treat arrhythmias. Continuous electrocardiogram (ECG) monitoring helps in assessing the effectiveness of the drug in controlling arrhythmias and detecting any new or worsening arrhythmias that may require immediate attention.
Title: Choice E Reason:
Monitoring urine output is important because amiodarone can affect renal function, especially in patients with pre-existing kidney conditions. Keeping track of urine output helps in assessing renal function and ensuring that the drug is not causing nephrotoxicity
Correct Answer is A
Explanation
Choice A Reason:
Assessing the client’s gag reflex before giving any food or water is crucial after a bronchoscopy. The procedure involves the use of local anesthesia to numb the throat, which can impair the gag reflex and increase the risk of aspiration. Ensuring that the gag reflex has returned before allowing the client to eat or drink helps prevent choking and aspiration, which are serious complications.
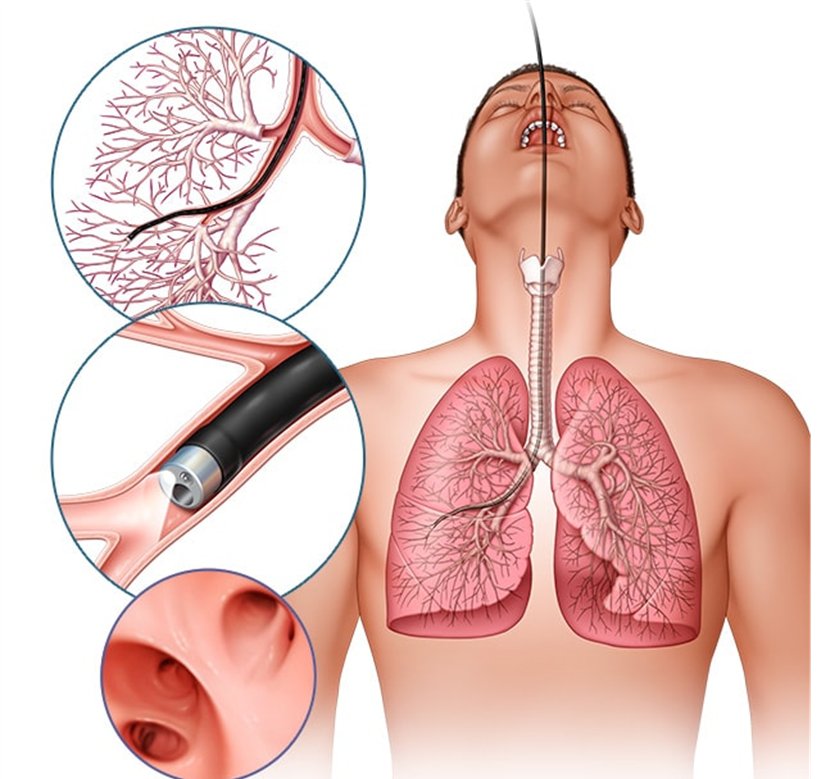
Choice B Reason:
Providing the client with ice chips instead of a drink of water is not the best initial action. While ice chips may seem like a safer option, they still pose a risk of aspiration if the gag reflex has not fully returned. The priority is to first assess the gag reflex to ensure the client can safely swallow.
Choice C Reason:
Contacting the primary healthcare provider and getting the appropriate orders is not necessary as the first action. The nurse can independently assess the gag reflex, which is a standard nursing practice after procedures involving throat anesthesia. If there are concerns after the assessment, then contacting the healthcare provider would be appropriate.
Choice D Reason:
Letting the client have a small sip to evaluate the ability to swallow is not safe without first assessing the gag reflex. This approach could lead to aspiration if the gag reflex has not returned. The initial step should always be to assess the gag reflex to ensure the client can safely swallow liquids.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
