A nurse is assessing a client who has fluid overload. Which of the following findings should the nurse expect? (Select all that apply)
Increased temperature
Increased respiratory rate
Increased hematocrit
Increased heart rate
Increased blood pressure
Correct Answer : A,B,C
Choice A: Increased Respiratory Rate
Fluid overload, also known as hypervolemia, can lead to an increased respiratory rate. This occurs because the excess fluid in the body can accumulate in the lungs, leading to pulmonary congestion and edema. As a result, the body attempts to compensate by increasing the respiratory rate to improve oxygenation and remove excess carbon dioxide. Normal respiratory rate for adults is typically between 12-20 breaths per minute. An increased respiratory rate above this range can indicate fluid overload.
Choice B: Increased Heart Rate
An increased heart rate, or tachycardia, is another common finding in clients with fluid overload. The heart has to work harder to pump the excess fluid throughout the body, leading to an increased heart rate. This is a compensatory mechanism to maintain adequate cardiac output and tissue perfusion. Normal resting heart rate for adults is between 60-100 beats per minute. A heart rate above this range can be indicative of fluid overload.
Choice C: Increased Blood Pressure
Fluid overload can also result in increased blood pressure, or hypertension. The excess fluid in the bloodstream increases the volume of blood that the heart has to pump, leading to higher pressure within the arteries. This can strain the cardiovascular system and lead to complications if not managed properly. Normal blood pressure is typically around 120/80 mmHg. Blood pressure readings consistently above this range can suggest fluid overload.
Choice D: Increased Hematocrit
Increased hematocrit is not typically associated with fluid overload. Hematocrit is the proportion of red blood cells in the blood. In cases of fluid overload, the hematocrit level is usually decreased due to the dilutional effect of the excess fluid. Therefore, this choice is incorrect.
Choice E: Increased Temperature
Increased temperature is not a common finding in fluid overload. Fever or elevated body temperature is more commonly associated with infections or inflammatory conditions. Fluid overload does not typically cause an increase in body temperature. Therefore, this choice is incorrect.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A reason:
Strict monitoring of hourly intake and output is important for managing fluid balance and detecting potential complications such as dehydration or fluid overload1. However, it is not the highest priority in the acute phase of bacterial meningitis. The primary concern is to monitor for signs of increased intracranial pressure (ICP) and neurological deterioration.
Choice B reason:
Managing pain through drug and non-drug methods is essential for patient comfort and overall well-being. Pain management can help reduce stress and improve the patient’s ability to rest and recover. However, it is not the highest priority compared to monitoring neurological status, which can provide early indications of complications such as increased ICP or seizures.
Choice C reason:
Assessing neurological status at least every 2 to 4 hours is the highest priority for a client with bacterial meningitis. This frequent assessment helps detect early signs of neurological deterioration, increased ICP, and other complications. Early detection and intervention are crucial in preventing severe outcomes and improving the patient’s prognosis.
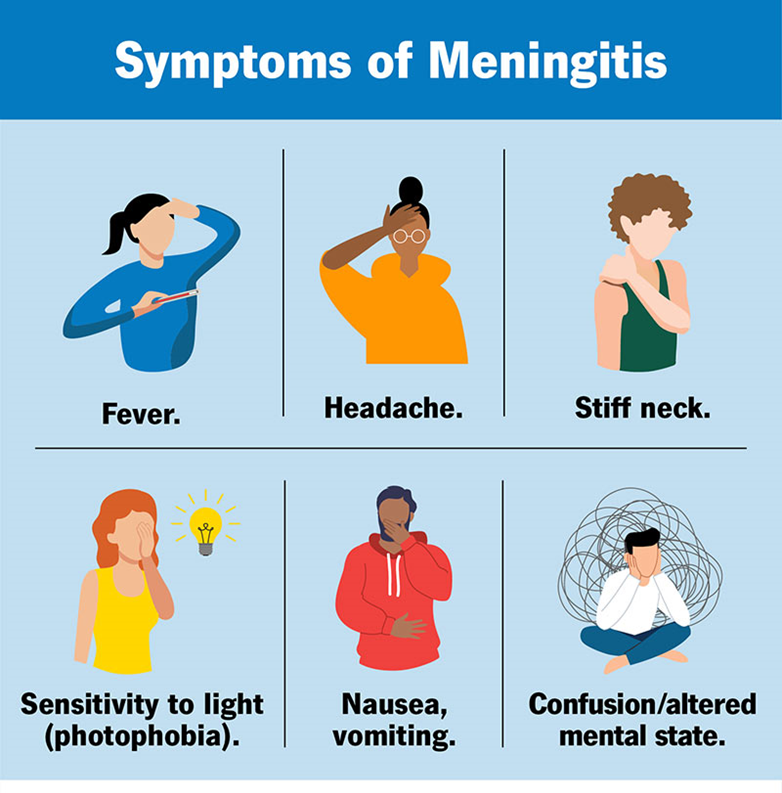
Choice D reason:
Decreasing environmental stimuli is important to reduce stress and prevent exacerbation of symptoms such as headache and photophobia. While this intervention is beneficial, it is not as critical as frequent neurological assessments in the acute management of bacterial meningitis.
Correct Answer is ["C","E"]
Explanation
Choice A: Formed stool in collection pouch
Formed stool in the collection pouch is not expected in an ileostomy. The output from an ileostomy is typically liquid to semi-liquid because the ileum does not absorb as much water as the colon. If formed stool is present, it may indicate a blockage or other issue that needs to be addressed.
Choice B: Stoma is edematous and bleeding
An edematous and bleeding stoma is not a normal finding and may indicate complications such as infection, trauma, or poor stoma care. The stoma should be moist and pink, but not swollen or bleeding. Persistent bleeding or significant edema should be reported to a healthcare provider immediately.
Choice C: Stoma is pink and shiny
A pink and shiny stoma is a sign that the ileostomy is functioning well. This indicates good blood flow and healthy tissue. The stoma should always appear moist and pink, similar to the inside of the mouth. Any deviation from this appearance, such as a pale, dark, or dry stoma, should be evaluated by a healthcare professional.
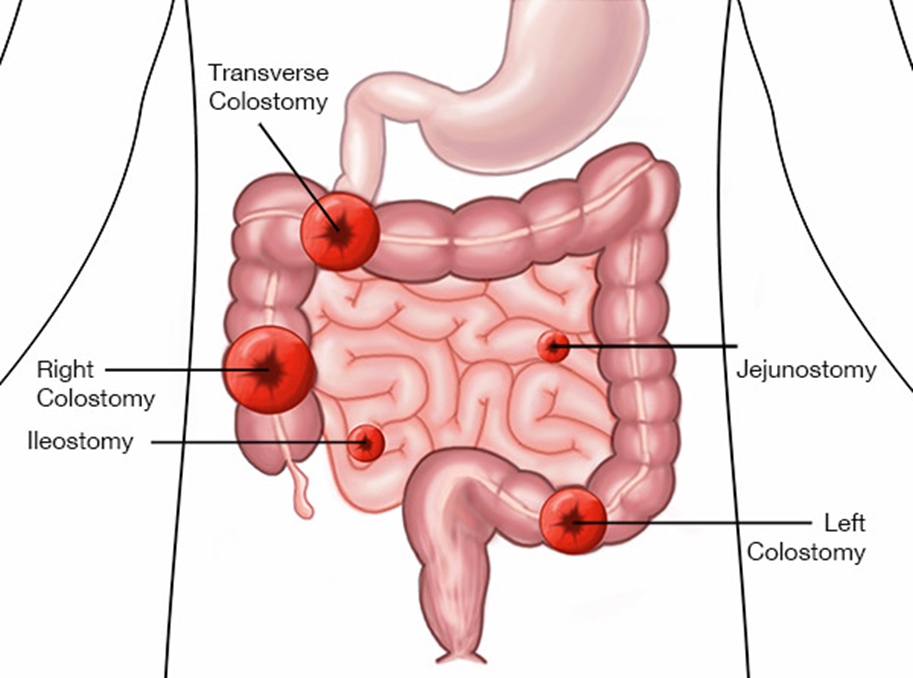
Choice D: Skin excoriation around the stoma
Skin excoriation around the stoma is not a normal finding and suggests that the skin is being irritated by the stoma output or the ostomy appliance. Proper skin care and fitting of the ostomy appliance are essential to prevent skin breakdown. If excoriation occurs, it should be treated promptly to prevent further complications.
Choice E: Mucus liquid flows from the stoma
Mucus liquid flowing from the stoma is expected in an ileostomy. The output is typically liquid to semi-liquid and may contain mucus, which is normal for the small intestine. This type of output indicates that the ileostomy is functioning as intended.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
