A nurse in a PACU is assessing a client who has a newly created colostomy. Which of the following findings should the nurse report to the provider?
Rosebud-like stoma orifice
Stoma oozing red drainage
Shiny, moist stoma
Purplish-colored stoma
None
None
The Correct Answer is D
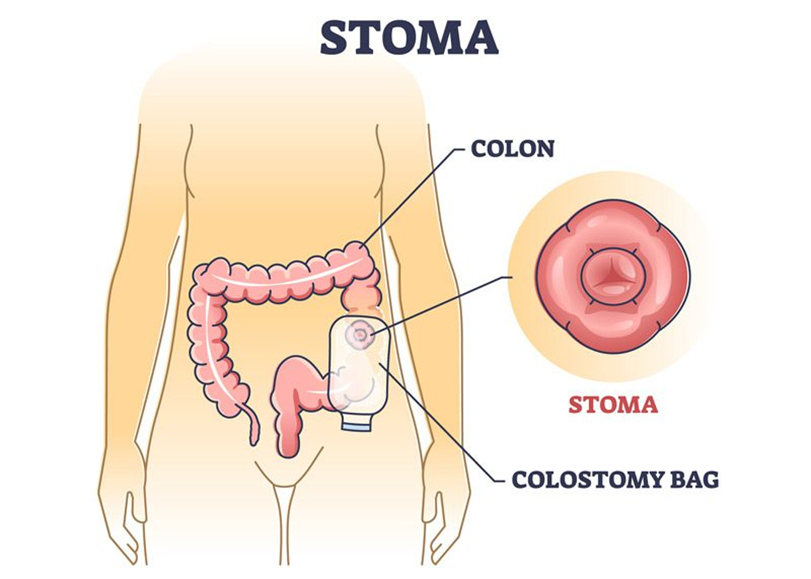
Choice A: Rosebud-like Stoma Orifice
A rosebud-like stoma orifice is typically a normal appearance for a new stoma. The stoma should be moist, pink to red in color, and protrude slightly from the abdomen, resembling a rosebud. This appearance indicates good blood flow and proper healing. Therefore, this finding does not usually require immediate reporting to the provider.
Choice B: Stoma Oozing Red Drainage
While some minor bleeding or oozing can be normal immediately after surgery, persistent or significant red drainage from the stoma could indicate a complication such as infection or trauma to the stoma site. This finding should be monitored closely, but it is not as immediately concerning as a purplish-colored stoma, which indicates a more severe issue.
Choice C: Shiny, Moist Stoma
A shiny, moist stoma is a sign of a healthy stoma. The stoma should always appear moist and slightly shiny due to the mucus produced by the intestinal lining. This finding is normal and does not require reporting to the provider.
Choice D: Purplish-Colored Stoma
A purplish-colored stoma is an immediate concern and should be reported to the provider. This discoloration can indicate compromised blood flow to the stoma, which can lead to tissue necrosis if not addressed promptly. Ensuring adequate blood supply is crucial for the stoma’s viability and the patient’s overall health. Immediate medical intervention is necessary to prevent further complications.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Provide a quiet, low-stimulus environment
Choice A Reason:
Provide a quiet, low-stimulus environment
This is the correct answer. A quiet, low-stimulus environment helps to reduce the metabolic demands on the body and prevent overstimulation, which can trigger a thyroid crisis. Hyperthyroidism increases the body’s metabolic rate, and excessive stimulation can exacerbate symptoms and lead to a crisis. Therefore, creating a calm environment is crucial in managing hyperthyroidism and preventing complications.
Choice B Reason:
Keep the client NPO
Keeping the client NPO (nothing by mouth) is not typically necessary for preventing a thyroid crisis. While it may be required for certain procedures or if the client is experiencing severe symptoms, it is not a standard intervention for hyperthyroidism management. Therefore, this choice is not correct.
Choice C Reason:
Administer aspirin as prescribed for any sign of hyperthermia
Administering aspirin for hyperthermia is not recommended in clients with hyperthyroidism. Aspirin can increase free thyroid hormone levels by displacing thyroid hormones from their binding proteins, potentially worsening hyperthyroidism. Instead, other antipyretics like acetaminophen are preferred. Therefore, this choice is not correct.
Choice D Reason:
Observe the client carefully for signs of hypocalcemia
Observing for signs of hypocalcemia is not directly related to preventing a thyroid crisis. Hypocalcemia is more commonly associated with thyroidectomy or parathyroidectomy rather than hyperthyroidism itself. Therefore, this choice is not correct.
Correct Answer is D
Explanation
Choice A reason: No change to the heparin rate is not appropriate in this scenario. The normal range for PTT is generally between 25 to 35 seconds. However, for a client on heparin therapy, the target PTT is typically 1.5 to 2.5 times the normal range, which would be approximately 60 to 80 seconds. Since the client’s PTT is only 25 seconds, it indicates that the blood is clotting too quickly, and the heparin dose is insufficient.
Choice B reason: Decreasing the heparin rate would further reduce the anticoagulant effect, which is not advisable given the current PTT of 25 seconds. Lowering the heparin rate could increase the risk of thrombus formation and worsen the deep vein thrombosis (DVT) condition.
Choice C reason: Stopping heparin and starting warfarin is not an immediate solution. Warfarin takes several days to achieve its full anticoagulant effect, and during this transition period, the client would be at risk of clot formation. Heparin provides immediate anticoagulation, which is crucial in the acute management of DVT.
Choice D reason: Increasing the heparin rate is the correct action. The current PTT of 25 seconds is below the therapeutic range for a client on heparin therapy. Increasing the heparin rate will help achieve the desired anticoagulant effect, prolonging the PTT to the target range of 60 to 80 seconds.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
