A nurse is providing dietary teaching for a client who has Cushing’s disease. Which of the following recommendations should the nurse include in the teaching?
Decrease protein intake.
Restrict sodium intake.
Limit intake of potassium-rich foods.
Increase carbohydrate intake.
The Correct Answer is B
Choice A Reason:
Decrease protein intake: This is not typically recommended for clients with Cushing’s disease. Protein is essential for maintaining muscle mass and overall health. Clients with Cushing’s disease often experience muscle weakness and wasting, so adequate protein intake is crucial to help counteract these effects. Therefore, decreasing protein intake would not be beneficial.
Choice B Reason:
Restrict sodium intake: Clients with Cushing’s disease often suffer from hypertension (high blood pressure) due to the excess cortisol in their bodies. High sodium intake can exacerbate this condition by increasing blood pressure even further. Therefore, it is crucial to restrict sodium intake to help manage hypertension and reduce the risk of cardiovascular complications. Foods high in sodium include processed foods, canned soups, and salty snacks. The recommended daily sodium intake for most adults is less than 2,300 milligrams, but for those with hypertension, it is often advised to consume even less.
Choice C Reason:
Limit intake of potassium-rich foods: This is not a standard recommendation for clients with Cushing’s disease. In fact, potassium is often beneficial as it can help counteract the effects of sodium and lower blood pressure. Potassium-rich foods include bananas, oranges, spinach, and sweet potatoes. Limiting these foods would not be advantageous and could potentially worsen hypertension.
Choice D Reason:
Increase carbohydrate intake: Increasing carbohydrate intake is not typically recommended for clients with Cushing’s disease. Excess cortisol can lead to increased blood sugar levels and a higher risk of developing diabetes. Therefore, it is important to manage carbohydrate intake carefully to avoid spikes in blood sugar. Instead, a balanced diet with a focus on complex carbohydrates, lean proteins, and healthy fats is recommended.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
The correct answer is a) 1 cup of milk.
Choice A reason: One cup of milk contains approximately 15 grams of carbohydrates. Milk is a good source of carbohydrates, protein, and calcium, making it a suitable option for maintaining blood glucose levels during exercise. It is important for individuals with diabetes to monitor their carbohydrate intake to manage their blood sugar levels effectively.
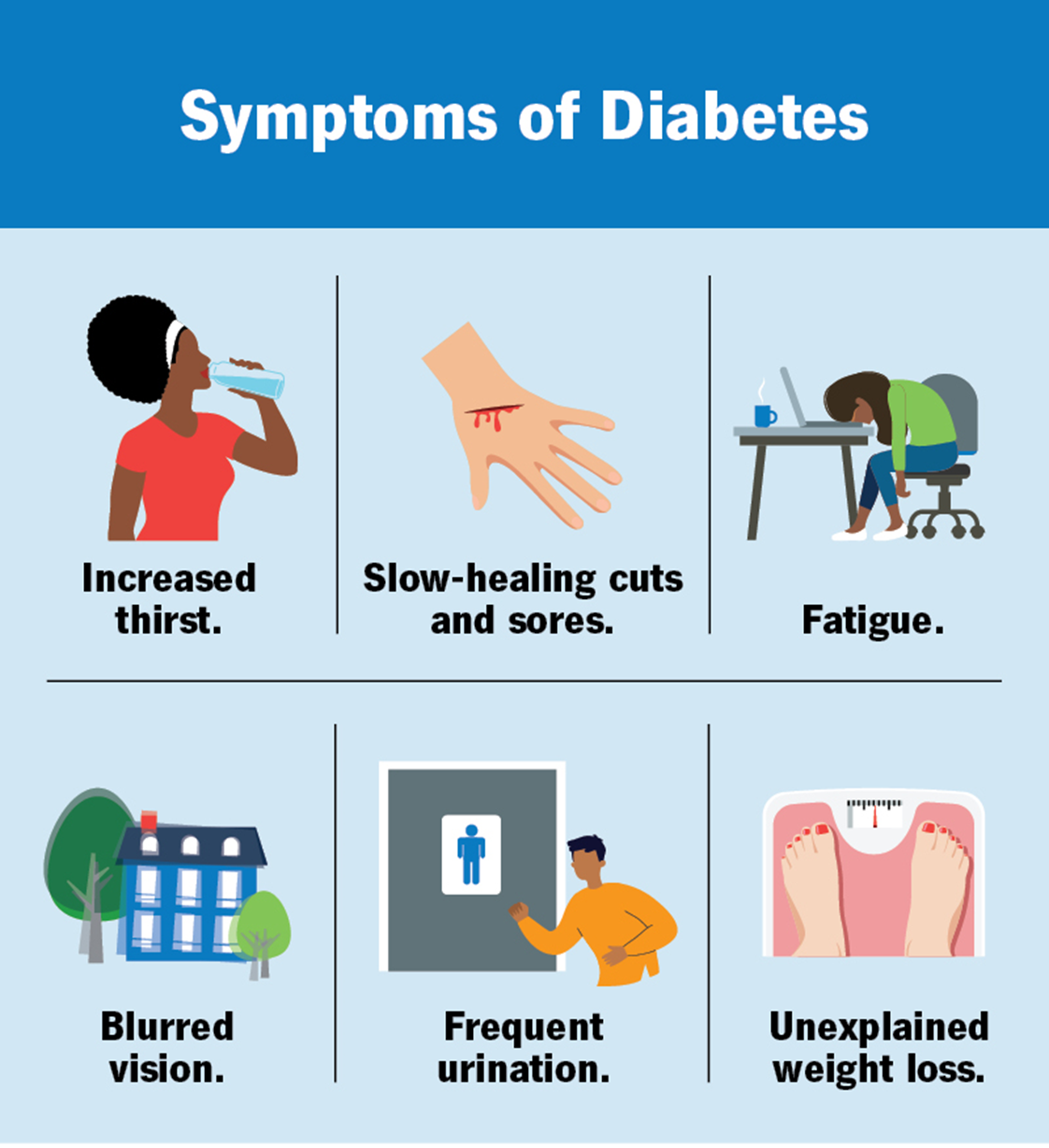
Choice B reason: Half a cup of regular ice cream contains around 15 grams of carbohydrates. However, ice cream also contains high levels of sugar and fat, which may not be the healthiest option for regular consumption, especially for individuals with diabetes. While it can be included occasionally, it is better to choose healthier carbohydrate sources.
Choice C reason: One slice of bread typically contains about 15 grams of carbohydrates. Bread, especially whole grain or whole wheat varieties, can be a good source of carbohydrates for individuals with diabetes. It provides fiber, which helps in maintaining stable blood sugar levels.
Choice D reason: One cup of sugar-free yogurt does not contain 15 grams of carbohydrates. Sugar-free yogurt usually has fewer carbohydrates compared to regular yogurt. It is important to read the nutritional labels to determine the exact carbohydrate content. Regular yogurt, on the other hand, can be a good source of carbohydrates.
Correct Answer is ["A","B","C","D"]
Explanation
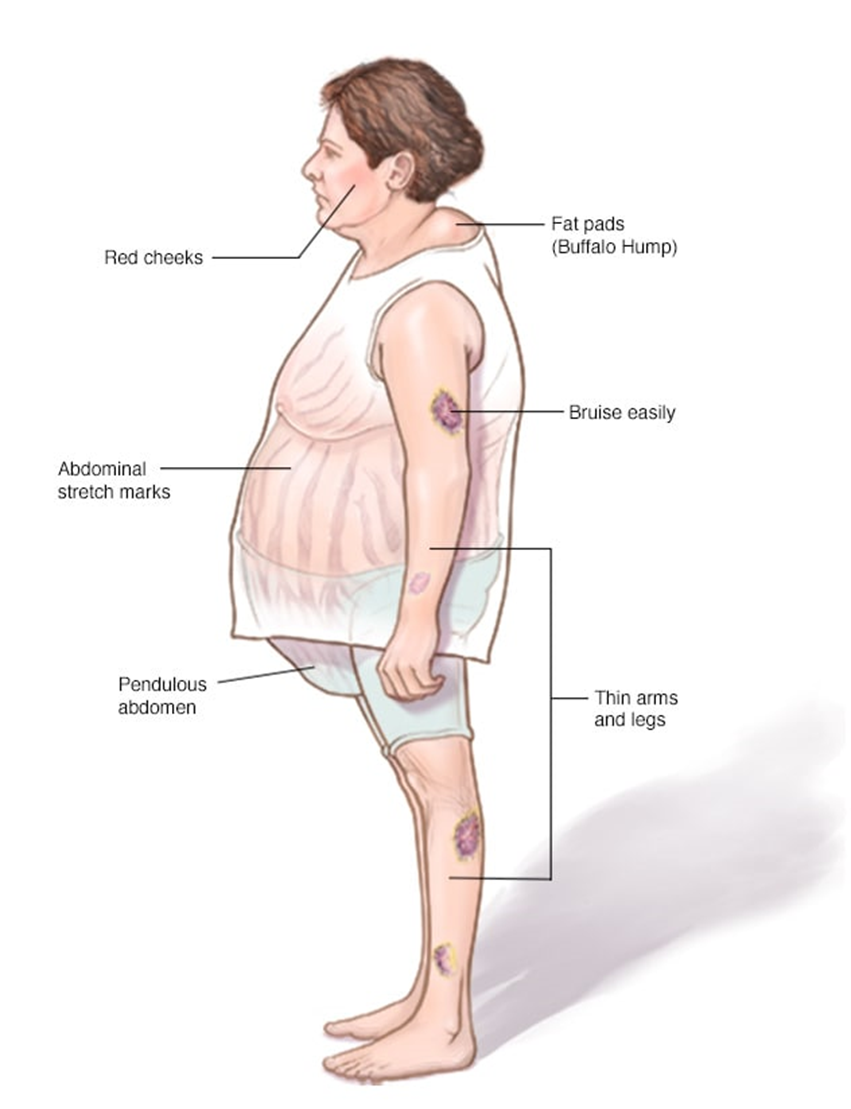
Choice A reason: A buffalo hump is a characteristic sign of Cushing’s syndrome. It refers to the accumulation of fat on the back of the neck and shoulders. This symptom occurs due to the excessive production of cortisol, which leads to abnormal fat distribution in the body.
Choice B reason: Moon face is another hallmark of Cushing’s syndrome. It describes the rounding and fullness of the face, which results from fat deposits. This symptom is also caused by prolonged exposure to high levels of cortisol.
Choice C reason: Hypertension, or high blood pressure, is commonly associated with Cushing’s syndrome. Cortisol increases blood pressure by enhancing the sensitivity of blood vessels to catecholamines and by promoting sodium and water retention.
Choice D reason: Purple striations, or stretch marks, are often seen in individuals with Cushing’s syndrome. These marks typically appear on the abdomen, thighs, breasts, and arms. They result from the thinning of the skin and the breakdown of collagen due to elevated cortisol levels.
Choice E reason: Tremors are not typically associated with Cushing’s syndrome. While Cushing’s syndrome can cause a variety of symptoms, tremors are more commonly linked to other conditions such as hyperthyroidism or neurological disorders.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
