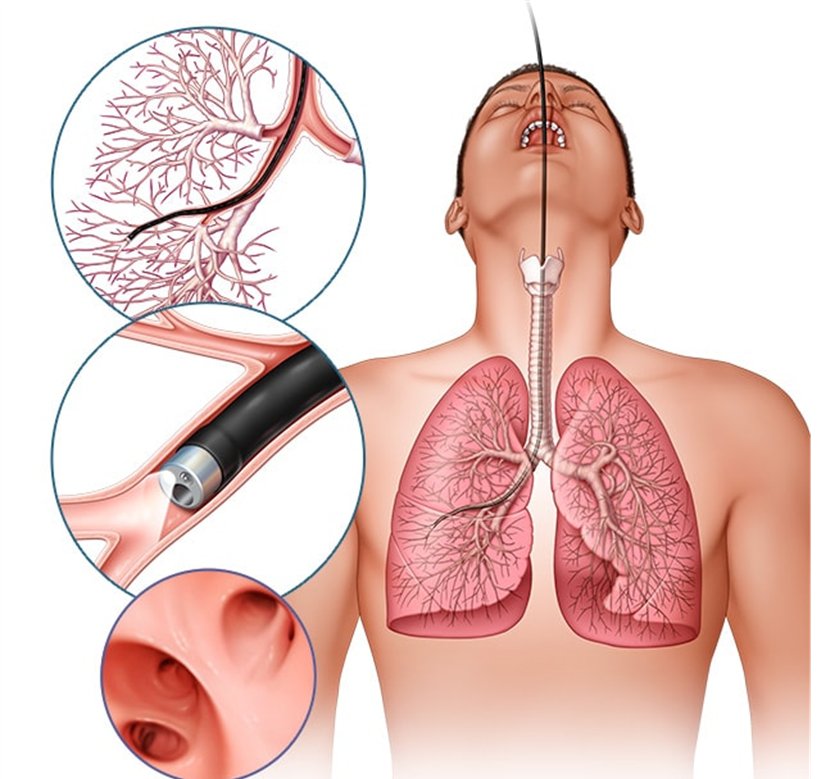
A client who had a bronchoscopy 2 hours ago asks for a drink of water. What action would the nurse take initially to assure client safety?
Assess the client’s gag reflex before giving any food or water.
Provide the client with ice chips instead of a drink of water.
Contact the primary healthcare provider and get the appropriate orders.
Let the client have a small sip to evaluate the ability to swallow.
The Correct Answer is A
Choice A Reason:
Assessing the client’s gag reflex before giving any food or water is crucial after a bronchoscopy. The procedure involves the use of local anesthesia to numb the throat, which can impair the gag reflex and increase the risk of aspiration. Ensuring that the gag reflex has returned before allowing the client to eat or drink helps prevent choking and aspiration, which are serious complications.
Choice B Reason:
Providing the client with ice chips instead of a drink of water is not the best initial action. While ice chips may seem like a safer option, they still pose a risk of aspiration if the gag reflex has not fully returned. The priority is to first assess the gag reflex to ensure the client can safely swallow.
Choice C Reason:
Contacting the primary healthcare provider and getting the appropriate orders is not necessary as the first action. The nurse can independently assess the gag reflex, which is a standard nursing practice after procedures involving throat anesthesia. If there are concerns after the assessment, then contacting the healthcare provider would be appropriate.
Choice D Reason:
Letting the client have a small sip to evaluate the ability to swallow is not safe without first assessing the gag reflex. This approach could lead to aspiration if the gag reflex has not returned. The initial step should always be to assess the gag reflex to ensure the client can safely swallow liquids.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["B","C"]
Explanation
Choice A Reason: High-flow nasal cannula
The high-flow nasal cannula (HFNC) is designed to deliver oxygen at flow rates much higher than 5 liters per minute, typically ranging from 20 to 60 liters per minute. It is used for patients requiring high levels of oxygen and positive airway pressure. Therefore, it is not appropriate for a flow rate of 5 liters per minute.
Choice B Reason: Simple face mask
The simple face mask is suitable for delivering oxygen at flow rates between 6 to 10 liters per minute. However, it can also be used at a flow rate of 5 liters per minute, providing an FiO2 (fraction of inspired oxygen) of approximately 40-60%. This makes it an appropriate choice for the given requirement.
Choice C Reason: Nasal cannula
The nasal cannula is a low-flow oxygen delivery device that can deliver oxygen at flow rates from 1 to 6 liters per minute. At 5 liters per minute, it provides an FiO2 of approximately 40%. It is comfortable for patients and is commonly used for those who need a moderate amount of supplemental oxygen.
Choice D Reason: Non-rebreather mask
The non-rebreather mask is designed to deliver high concentrations of oxygen, typically at flow rates of 10 to 15 liters per minute. It is used in situations where patients need a high FiO2, close to 100%. Therefore, it is not suitable for a flow rate of 5 liters per minute.
Choice E Reason: Venturi mask
The Venturi mask is used to deliver precise oxygen concentrations, typically ranging from 24% to 60% FiO2. It is suitable for patients who require controlled oxygen therapy. While it can be adjusted to deliver oxygen at a flow rate of 5 liters per minute, it is generally used for more specific FiO2 requirements.
Correct Answer is D
Explanation
Choice A Reason:
Malfunction of the alarm button is unlikely to be the cause of increased peak airway pressure. The alarm is designed to alert the nurse to a problem with the ventilator or the patient’s airway, not to malfunction itself. Therefore, this is not the first thing the nurse should assess.
Choice B Reason:
A cut or slice in the tubing from the ventilator could cause a loss of pressure or air leak, but it would not typically result in increased peak airway pressure. Instead, it would likely cause a decrease in pressure and potentially trigger a different alarm.
Choice C Reason:
Higher than normal endotracheal cuff pressure can contribute to increased peak airway pressure. However, it is not the most immediate concern compared to a kink in the tubing, which can completely obstruct airflow and rapidly compromise the patient’s ventilation.
Choice D Reason:
A kink in the ventilator tubing is a common and immediate cause of increased peak airway pressure. It obstructs the flow of air, leading to a buildup of pressure in the system. This is the first thing the nurse should assess and correct to ensure the patient is receiving adequate ventilation.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
