A patient is admitted for pain in the arm and jaw. The patient is later diagnosed with angina.
What type of pain does the arm and jaw pain most likely represent?
Intractable
Phantom
Referred
Cramping
The Correct Answer is C
Choice A rationale:
Intractable pain is pain that is persistent and does not respond to usual pain management methods. While angina can be intractable in some cases, it does not typically manifest as pain in the arm and jaw. Moreover, the patient in this scenario has not yet undergone pain management efforts, so it's premature to classify the pain as intractable.
Choice B rationale:
Phantom pain is pain that is felt in a part of the body that has been amputated or is no longer there. The patient in this scenario has not experienced any amputations, so phantom pain is not a valid explanation for the arm and jaw pain.
Choice C rationale:
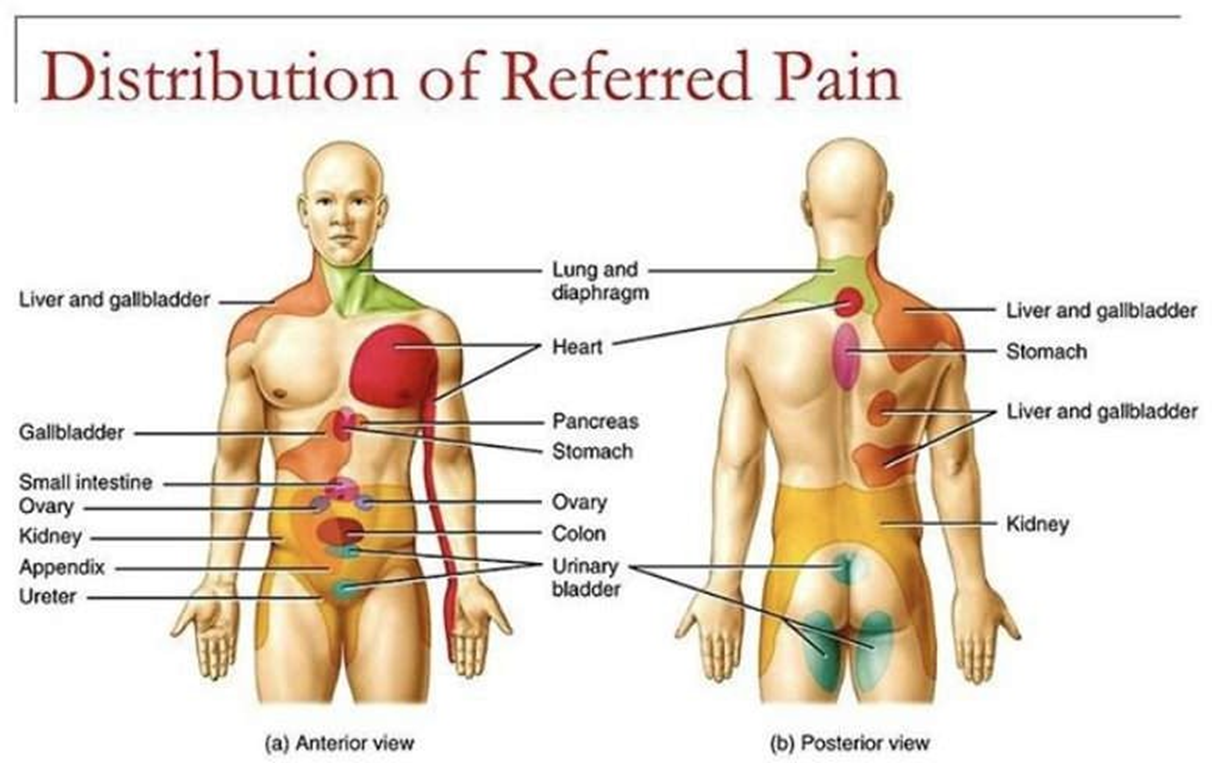
Referred pain is pain that is felt in a part of the body that is different from the source of the pain. This is the most likely explanation for the arm and jaw pain in this patient. The heart and the arm and jaw share nerve pathways, so pain signals from the heart can be misinterpreted by the brain as coming from these other areas. This is a common phenomenon in patients with angina.
Choice D rationale:
Cramping pain is a type of pain that is often described as a muscle tightening or squeezing sensation. It is not typically associated with angina. While angina can sometimes cause chest tightness, it's not characterized by cramping in the arm and jaw.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
The correct answer is Choice A.
Choice A rationale: Encouraging increased fluid intake helps maintain blood volume and reduces viscosity, promoting circulation and lowering the risk of venous stasis and clot formation postoperatively.
Choice B rationale: Keeping the affected knee flexed impairs venous return and increases stasis, elevating the risk of thrombosis. Proper positioning with extension promotes circulation and reduces clot risk.
Choice C rationale: Prolonged bed rest contributes to immobility-induced venous stasis, a major risk factor for DVT. Early ambulation and leg exercises are essential to prevent thromboembolic events.
Choice D rationale: Massaging the calf of a postoperative patient is contraindicated due to the risk of dislodging a thrombus, potentially leading to a life-threatening pulmonary embolism.
Correct Answer is B
Explanation
Choice A rationale:
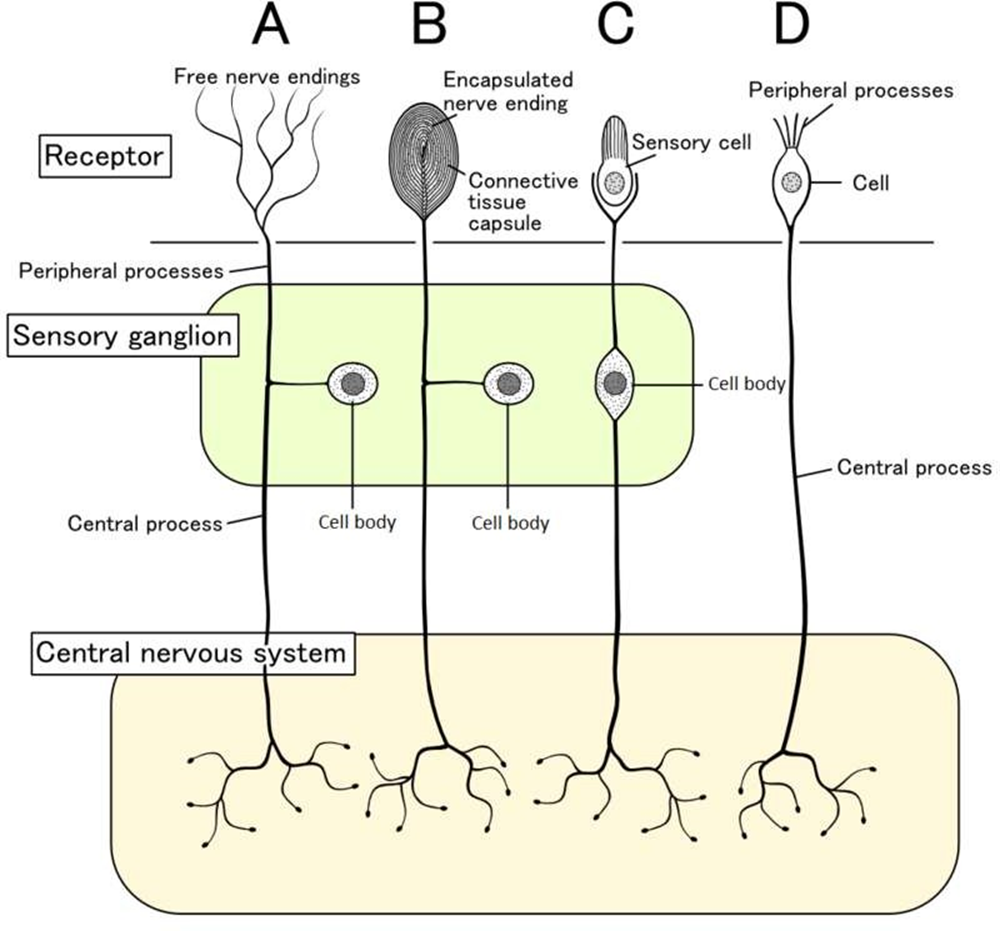
The spinal cord plays a crucial role in pain transmission, but it does not initiate the afferent pathways. It receives pain signals from nociceptors and relays them to the brain for processing.
The spinal cord is also involved in pain modulation, as it can dampen or amplify pain signals depending on various factors. However, it is not the primary trigger for pain sensation. That role belongs to nociceptors.
Choice B rationale:
Nociceptors are specialized sensory receptors that detect potentially damaging stimuli, such as intense heat, pressure, or chemical irritants.
They are located throughout the body, including the skin, muscles, joints, and internal organs.
When nociceptors are activated, they generate electrical signals that travel along nerve fibers to the spinal cord and brain. This process initiates the afferent pathways, which ultimately lead to the conscious perception of pain.
Nociceptors are essential for protecting the body from harm. They alert us to potential dangers and trigger responses that help us avoid injury or further damage.
Choice C rationale:
Endorphins are natural pain-relieving substances produced by the body. They act on receptors in the brain and spinal cord to reduce pain perception.
However, endorphins do not trigger the afferent pathways. They work by modulating pain signals that have already been initiated by nociceptors.
Choice D rationale:
The cortex is the outer layer of the brain that is responsible for higher-level functions, such as thinking, feeling, and decision- making.
It plays a role in the conscious experience of pain, but it does not trigger the afferent pathways.
The cortex receives pain signals from the spinal cord and processes them, leading to the awareness of pain.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
