An elderly client is 12-hours postoperative for a hernia repair and suddenly becomes agitated, staggers out into the corridor, and demands to be set free.
After assisting the client back to bed and administering pain medication, which intervention is best for the practical nurse (PN) to implement?
Administer a prescribed narcotic antagonist to reverse the effects of any analgesic accumulation
Notify the healthcare provider and request a prescription for restraints to minimize the client's danger to self.
Raise the side rails and notify the family to come and stay until the client is reoriented and cooperative
Instruct a UAP to keep the upper side rails up and check on the client every 15 minutes until the client is resting.
The Correct Answer is C
The correct answer is c. Raise the side rails and notify the family to come and stay until the client is reoriented and cooperative. This intervention ensures the client’s safety and provides familiar support, which can help reorient and calm the client.
Choice A reason: Administering a prescribed narcotic antagonist assumes the agitation is due to narcotic accumulation without evidence. This could lead to unnecessary medication administration.
Choice B reason: Requesting restraints should be a last resort due to the risks of injury and increased agitation. Restraints can also lead to further complications.
Choice C reason: Raising the side rails and involving the family provides immediate safety and emotional support, which can help reorient the client. Familiar faces can be very calming and reassuring.
Choice D reason: Instructing a UAP to check on the client every 15 minutes lacks the immediate family support that can help reorient the client. Continuous monitoring is important, but family involvement is more effective.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
A) Incorrect- Pupillary response is not relevant to the assessment of mesalamine's effectiveness.
Pupillary response is often assessed in neurological or ophthalmic evaluations and is not a direct measure of gastrointestinal function or the response to mesalamine therapy.
B) Incorrect- Peripheral pulses are not directly affected by mesalamine therapy, and monitoring them would not provide insight into the medication's effectiveness. Peripheral pulses are typically assessed to evaluate circulatory status and are not specific to the evaluation of gastrointestinal conditions.
C) Correct- Mesalamine is a medication commonly used to treat inflammatory bowel disease (IBD), such as Crohn's disease and ulcerative colitis. It helps to reduce inflammation in the gastrointestinal tract. Monitoring bowel patterns is important to assess the effectiveness of mesalamine in managing the symptoms of these conditions.
D) Incorrect- Oxygen saturation is a measure of the amount of oxygen in the blood and is used to assess respiratory function. While oxygen saturation is important for overall patient assessment, it is not directly related to mesalamine's effectiveness in treating inflammatory bowel disease.
Correct Answer is A
Explanation
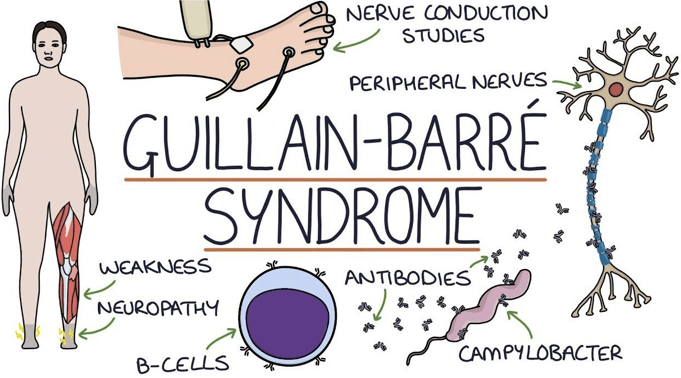
This is the finding that the PN should report to the charge nurse because it indicates a possible complication of Guillain-Barre syndrome, which is autonomic dysfunction. This can affect the cardiac, respiratory, and gastrointestinal systems and cause life-threatening problems such as arrhythmias, hypotension, or respiratory failure. The PN should monitor the client's vital signs closely and report any abnormal changes.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
