A client is receiving mesalamine 800 mg by mouth three times a day. Which assessment should the nurse perform to assess the effectiveness of the medication?
Pupillary response.
Peripheral pulses.
Bowel patterns.
Oxygen saturation.
The Correct Answer is C
A) Incorrect- Pupillary response is not relevant to the assessment of mesalamine's effectiveness.
Pupillary response is often assessed in neurological or ophthalmic evaluations and is not a direct measure of gastrointestinal function or the response to mesalamine therapy.
B) Incorrect- Peripheral pulses are not directly affected by mesalamine therapy, and monitoring them would not provide insight into the medication's effectiveness. Peripheral pulses are typically assessed to evaluate circulatory status and are not specific to the evaluation of gastrointestinal conditions.
C) Correct- Mesalamine is a medication commonly used to treat inflammatory bowel disease (IBD), such as Crohn's disease and ulcerative colitis. It helps to reduce inflammation in the gastrointestinal tract. Monitoring bowel patterns is important to assess the effectiveness of mesalamine in managing the symptoms of these conditions.
D) Incorrect- Oxygen saturation is a measure of the amount of oxygen in the blood and is used to assess respiratory function. While oxygen saturation is important for overall patient assessment, it is not directly related to mesalamine's effectiveness in treating inflammatory bowel disease.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
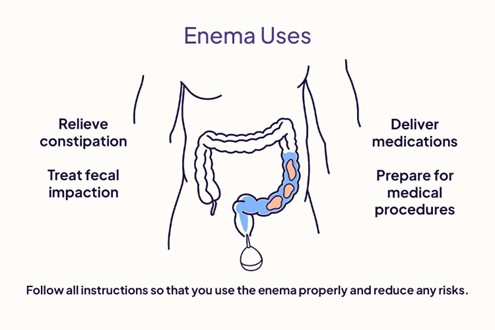
- An oil retention enema is used to soften the stool and lubricate the rectum, making it easier to pass the stool. It is usually oil-based and contains 90-120 ml of solution.
- The temperature of the enema solution affects the effectiveness and comfort of the procedure. If the solution is too hot or cold, it can cause pain, cramps, or damage to the rectal tissue³. If the solution is too warm, it can also stimulate peristalsis and cause the client to expel the enema before it has time to work.
- The ideal temperature for an enema solution is close to the client’s body temperature, which is around 98°F or 36°C. This temperature ensures that the solution is comfortable and does not cause adverse reactions.
Option A is incorrect because the client’s comfort level may not reflect the optimal temperature for the enema.
Option B is incorrect because the temperature of the enema does affect its effectiveness and safety.
Option D is incorrect because the temperature is too high and can cause harm to the client.
Correct Answer is A
Explanation
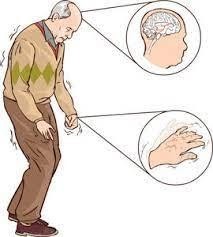
A) Correct- Clients with Parkinson's disease often experience bradykinesia and impaired mobility. Rising slowly from a seated position is important to prevent falls and maintain stability. Affirming the correct movement strategy promotes the client's safety.
B) Incorrect- Telling the UAP to make the client move more quickly could be unsafe and not appropriate for a client with Parkinson's disease. Rapid movements might lead to balance issues or falls.
C) Incorrect- While demonstrating proper technique might be helpful, it's not the most immediate action the nurse should take. The client's safety and well-being are the priority.
D) Incorrect- Painful movement is not the primary issue here. The client's movement is slow due to Parkinson's disease, and this is expected.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
