A nurse on a medical-surgical unit is assessing a client who has had a stroke. For which of the following findings should the nurse initiate a referral for occupational therapy?
Difficulty performing ADLs
Inability to swallow clear liquids
Elevated blood glucose levels
Unsteady gait when ambulating
The Correct Answer is A
- A. Correct. Difficulty performing ADLs such as dressing, grooming, bathing, or feeding may indicate that the client has impaired motor function, sensory perception, or cognitive ability due to the stroke, which can affect their independence and quality of life. Occupational therapy can help the client regain or adapt their skills and abilities for daily living.
- B. Incorrect. Inability to swallow clear liquids may indicate that the client has dysphagia or impaired swallowing function due to the stroke, which can increase their risk of aspiration and malnutrition. Speech therapy can help the client improve their swallowing function and provide recommendations for safe oral intake.
- C. Incorrect. Elevated blood glucose levels may indicate that the client has diabetes mellitus or impaired glucose metabolism due to the stroke, which can affect their healing and recovery process and increase their risk of complications such as infection or hyperglycemia/hypoglycemia episodes. Diabetes education and management can help the client control their blood glucose levels and prevent adverse outcomes.
- D. Incorrect. Unsteady gait when ambulating may indicate that the client has impaired balance, coordination, or muscle strength due to the stroke, which can affect their mobility and safety and increase their risk of falls or injuries. Physical therapy can help the client improve their gait and mobility and provide assistive devices if needed.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A rationale:
Telling the client, "It's not your choice to be here, so you have to accept the treatment we plan for you," disregards the client's autonomy and right to make decisions about their own healthcare. In mental health settings, respecting a patient's autonomy and involving them in the decision-making process is crucial for ethical care. This statement does not address the client's fear or provide any reassurance.
Choice B rationale:
Choice C rationale:
Asking, "Why do you think your provider will prescribe you medications that will make you sleep?" attempts to explore the client's fear, but it may come across as dismissive or invalidating. It could make the client feel unheard or misunderstood, which is not ideal in this situation.
Choice D rationale:
Stating, "I will make sure that we respect your right to refuse medications," is the most appropriate response. It acknowledges the client's fear and reassures them that their autonomy will be respected. It opens the door for a discussion about the client's concerns, allowing them to express their fears and preferences. Respecting the client's right to refuse medications is fundamental to ethical nursing practice and patient-centered care.
Correct Answer is B
Explanation
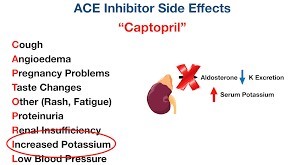
- A is incorrect because tinnitus, or ringing in the ears, is not an adverse effect of captopril, but rather a symptom of other conditions such as ear infection, noise exposure, or medication toxicity.
- B is correct because cough is a serious adverse effect of captopril, which is an angiotensinconverting enzyme (ACE) inhibitor that can cause angioedema, or swelling of the airways.
- C is incorrect because polyuria, or excessive urination, is not an adverse effect of captopril, but rather a symptom of other conditions such as diabetes mellitus, diabetes insipidus, or diuretic use.
- D is incorrect because blurred vision is not an adverse effect of captopril, but rather a symptom of other conditions such as eye strain, refractive error, or cataract.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
