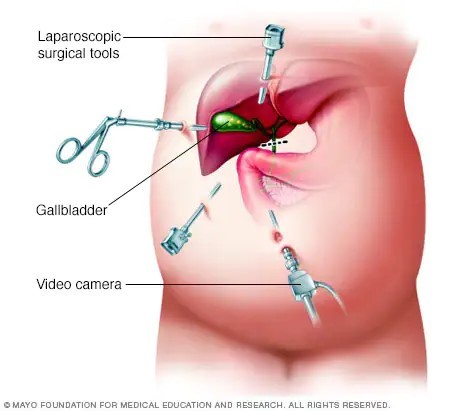
A nurse is reinforcing teaching with a client who is postoperative following a laparoscopic cholecystectomy. Which of the following statements by the client indicates an understanding of the teaching?
“I should eat a high-fat diet for several weeks."
"I should expect to have diarrhea until my diet changes."
"I should expect to have nausea for several days."
"I should leave my steri-strips on until they fall off."
The Correct Answer is D
After a laparoscopic cholecystectomy, steri-strips or adhesive strips are commonly placed over the small incisions. The client should keep the steri-strips in place until they fall off on their own or until they are removed by the healthcare provider during a follow-up visit. Removing the steri-strips prematurely can increase the risk of infection or disrupt the healing process.
"I should eat a high-fat diet for several weeks": After a laparoscopic cholecystectomy, it is important for the client to follow a low-fat diet initially to allow the body time to adjust to the absence of the gallbladder. High-fat foods can be more difficult to digest and may cause digestive discomfort. Gradually introducing small amounts of fat back into the diet is recommended, but a high-fat diet is not appropriate.
"I should expect to have diarrhea until my diet changes": While changes in bowel movements can occur after a cholecystectomy, such as looser stools or changes in frequency, persistent diarrhea is not expected or normal. If the client experiences persistent diarrhea, they should contact their healthcare provider for further evaluation.
"I should expect to have nausea for several days": While some clients may experience mild nausea or discomfort after the surgery, it should generally improve within a few days. If the client experiences persistent or severe nausea, they should contact their healthcare provider.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
"I should decrease my salt intake to 2 grams per day." - This statement is correct. Decreasing salt intake is an important dietary modification for individuals with hypertension. The general recommendation is to limit sodium intake to 2 grams per day or less. Reducing salt intake can help lower blood pressure levels.
"I can have two glasses of wine with dinner." - This statement is not accurate. While moderate alcohol consumption may have some health benefits, it is generally recommended to limit alcohol intake, especially for individuals with hypertension. The specific recommendation for alcohol consumption may vary depending on individual factors and should be discussed with a healthcare provider.
"I should exercise for 15 minutes two times per week." - This statement is not accurate. While any amount of physical activity is beneficial, the current recommendations for adults include at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity per week, along with muscle-strengthening activities on two or more days. The client should aim for a higher frequency and duration of exercise to achieve optimal health benefits.
Correct Answer is C
Explanation
When a charge nurse observes the smell of alcohol on a nurse's breath, it raises concerns about their ability to provide safe and competent care to clients. Patient safety is of utmost importance, and the charge nurse must take immediate action to address the situation.
Removing the nurse from the client care area ensures that the nurse is not involved in direct patient care while their ability to provide safe care is in question. This step helps mitigate potential risks to patient safety.
B and D- After removing the nurse from the client care area, further actions can be taken, such as documenting the objective findings about the situation and informing the supervisor. However, the immediate priority is to ensure patient safety by removing the nurse from the care area.
A- Assigning clients to the remaining staff can be done once the situation has been addressed and a suitable replacement for the nurse has been arranged.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
