A nurse is reinforcing teaching of a female client who has a family history of type 2 diabetes mellitus. The nurse should include which of the following risk factors for developing type 2 diabetes mellitus in the teaching?
Sedentary lifestyle
Triglyceride level of 100 mg/dL
Blood glucose of 98 mg/dL
Recent viral infection
The Correct Answer is A
Choice A: Sedentary lifestyle. This is a risk factor for developing type 2 diabetes mellitus, which is a condition that occurs when the body becomes resistant to the action of insulin or does not produce enough insulin to maintain normal blood glucose levels. Insulin is a hormone that helps glucose enter the cells and be used for energy. A sedentary lifestyle can increase the risk of type 2 diabetes mellitus by reducing physical activity, which can improve insulin sensitivity and lower blood glucose levels.
Choice B: Triglyceride level of 100 mg/dL. This is not a risk factor for developing type 2 diabetes mellitus, but rather a normal value. Triglycerides are a type of fat that circulates in the blood and can be used for energy or stored in adipose tissue. A high triglyceride level can indicate an increased risk of cardiovascular disease, but it is not directly related to type 2 diabetes mellitus.
Choice C: Blood glucose of 98 mg/dL. This is not a risk factor for developing type 2 diabetes mellitus, but rather a normal value. Blood glucose is the amount of glucose in the blood, which can vary depending on food intake, physical activity, and hormonal regulation. A high blood glucose level can indicate type 2 diabetes mellitus, but it is not a cause of it.
Choice D: Recent viral infection. This is not a risk factor for developing type 2 diabetes mellitus, but rather a possible trigger for type 1 diabetes mellitus, which is a condition that occurs when the immune system destroys the beta cells of the pancreas that produce insulin. A viral infection can trigger an autoimmune response that attacks the beta cells and causes type 1 diabetes mellitus.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
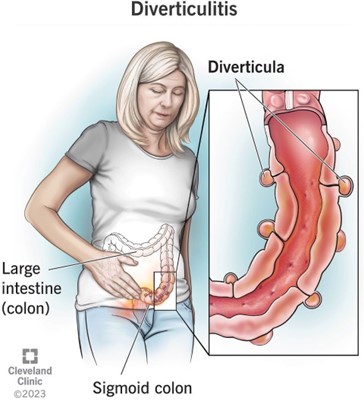
Choice A: Upper left quadrant. This is not the location where the nurse should expect the client to report abdominal pain who has diverticular disease. The upper left quadrant of the abdomen contains organs such as the stomach, spleen, pancreas, and part of the colon. Abdominal pain in this area can indicate conditions such as gastritis, peptic ulcer, pancreatitis, splenomegaly, or colon cancer.
Choice B: Lower left quadrant. This is the location where the nurse should expect the client to report abdominal pain who has diverticular disease, which is a condition that involves the formation of pouches or sacs in the wall of the colon. These pouches or sacs are called diverticula, and they can become inflamed or infected, causing diverticulitis. Diverticulitis can cause abdominal pain, fever, nausea, vomiting, and changes in bowel habits. The most common site of diverticula formation and diverticulitis is the sigmoid colon, which is located in the lower left quadrant of the abdomen.
Choice C: Upper right quadrant. This is not the location where the nurse should expect the client to report abdominal pain who has diverticular disease. The upper right quadrant of the abdomen contains organs such as the liver, gallbladder, duodenum, and part of the colon. Abdominal pain in this area can indicate conditions such as hepatitis, cholecystitis, duodenal ulcer, or colon cancer.
Choice D: Lower right quadrant. This is not the location where the nurse should expect the client to report abdominal pain who has diverticular disease. The lower right quadrant of the abdomen contains organs such as the appendix, cecum, and part of the colon. Abdominal pain in this area can indicate conditions such as appendicitis, Crohn’s disease, or colon cancer.
Correct Answer is D
Explanation
Choice A: Notify the nurse manager. This is an important action that the nurse should take, but not a priority. The nurse should notify the nurse manager to report the error and seek guidance on how to proceed. The nurse manager can also provide support and feedback to the nurse and help prevent similar errors in the future.
Choice B: Give the client 15 to 20 g of carbohydrate. This is a necessary action that the nurse should take, but not the priority. The nurse should give the client 15 to 20 g of carbohydrates to raise their blood glucose level and prevent or treat hypoglycemia. The nurse should choose a fast-acting carbohydrate source, such as juice, glucose tablets, or candy.
Choice C: Complete an incident report. This is a required action that the nurse should take, but not the priority. The nurse should complete an incident report to document the error and its consequences. The incident report can help identify the root cause of the error and improve patient safety and quality of care.
Choice D: Check the client’s blood glucose level. This is the priority action that the nurse should identify according to the ABCDE principle, which prioritizes interventions based on airway, breathing, circulation, disability, and exposure. The nurse should check the client’s blood glucose level to confirm the error and assess the risk of hypoglycemia, which is a low level of glucose in the blood. Hypoglycemia can cause symptoms such as sweating, trembling, confusion, and loss of consciousness. It can be life-threatening if not treated promptly.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
