A nurse is monitoring the pulmonary artery wedge pressure (PAWP) for a client. The nurse should identify that a reading of 17 mm Hg is an indication of which of the following conditions?
Right ventricular failure
Fluid volume deficit
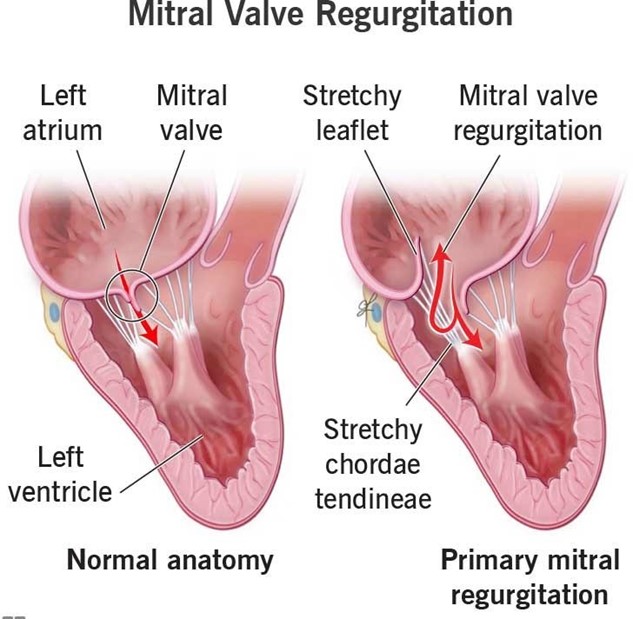
Mitral regurgitation
Afterload reduction
The Correct Answer is C
Choice A Reason: This is incorrect because right ventricular failure would cause an increase in right atrial pressure and right ventricular end-diastolic pressure, but not in PAWP, which reflects left atrial pressure and left ventricular end- diastolic pressure.
Choice B Reason: This is incorrect because fluid volume deficit would cause a decrease in PAWP, as there would be less blood volume in the pulmonary circulation.
Choice C Reason: This is correct because mitral regurgitation would cause an increase in PAWP, as the blood would back up into the left atrium and pulmonary veins due to the incompetent mitral valve.
Choice D Reason: This is incorrect because afterload reduction would cause a decrease in PAWP, as there would be less resistance to the left ventricular ejection and less blood volume in the pulmonary circulation.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A Reason: This is incorrect because a pneumothorax is a condition in which air enters the pleural space and causes the lung to collapse. It does not cause the chest wall to move inward and outward paradoxically.
Choice B Reason: This is incorrect because atelectasis is a condition in which alveoli collapse and cause reduced gas exchange. It does not cause the chest wall to move inward and outward paradoxically.
Choice C Reason: This is correct because flail chest is a condition in which multiple ribs are fractured and cause a segment of the chest wall to detach from the rest of the thoracic cage. It causes the chest wall to move inward and outward paradoxically, as well as dyspnea and pain.
Choice D Reason: This is incorrect because a hemothorax is a condition in which blood enters the pleural space and causes the lung to collapse. It does not cause the chest wall to move inward and outward paradoxically.
Correct Answer is B
Explanation
Choice A Reason: This choice is incorrect because urinary hesitancy is not the priority finding for the nurse to address.
Urinary hesitancy is a difficulty or delay in starting or maintaining a urine stream. It may be caused by various factors such as prostate enlargement, urinary tract infection, medication side effects, or psychological issues. It may cause discomfort, pain, or urinary retention, but it does not pose an immediate threat to the client's life.
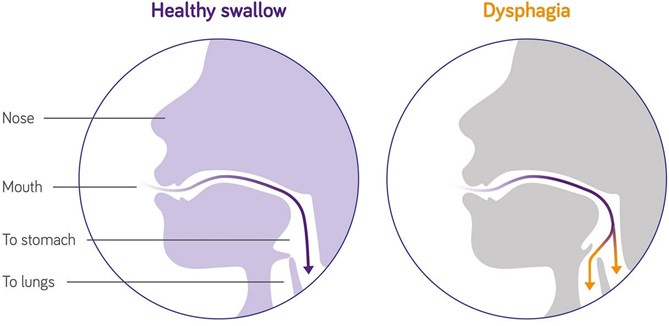
ChoiceB Reason: This choice is correct because dysphagia is the priority finding for the nurse to address. Dysphagia is a difficulty or inability to swallow food or liquids. It may be caused by various factors such as stroke, Parkinson's disease, dementia, esophageal cancer, or oral infections. It may cause malnutrition, dehydration, aspiration, or choking, which can lead to serious complications such as pneumonia, sepsis, or death. Therefore, the nurse should assess the client's swallowing function and provide appropriate interventions such as modifying the diet texture, using thickening agents, or teaching swallowing techniques.
ChoiceC Reason: This choice is incorrect because swollen gums are not the priority finding for the nurse to address. Swollen gums are an inflammation or enlargement of the gingival tissue that surrounds the teeth. They may be caused by various factors such as poor oral hygiene, gum disease, vitamin deficiency, medication side effects, or hormonal changes. They may cause bleeding, pain, or infection, but they do not pose an immediate threat to the client's life.
Choice D Reason: This choice is incorrect because pruritus is not the priority finding for the nurse to address. Pruritus is a sensation of itching that affects the skin. It may be caused by various factors such as dry skin, allergies, eczema, psoriasis, liver disease, or kidney disease. It may cause discomfort, scratching, or skin damage, but it does not pose an immediate threat to the client's life.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
