A nurse is caring for a patient with acute respiratory distress syndrome (ARDS) who is receiving mechanical ventilation using synchronized intermittent mandatory ventilation (SIMV). The settings include fraction of inspired oxygen (FIO2) of 80%, tidal volume of 450, rate of 16/minute, and positive end- expiratory pressure (PEEP) of 5 cm. Which assessment finding is most important for the nurse to report to the health care provider?
Respiratory rate 22 breaths/min
Heart rate 106 beats/min
02 saturation of 99%
Crackles audible at lung bases
The Correct Answer is D
D Crackles audible at the lung bases indicate the presence of pulmonary edema or fluid accumulation in the alveoli, which can compromise gas exchange and exacerbate respiratory distress. In a patient with ARDS, crackles suggest worsening pulmonary status and may indicate inadequate ventilation or oxygenation despite mechanical ventilation. Therefore, crackles at the lung bases are the most important finding to report to the healthcare provider as they may indicate a need for adjustments to the ventilator settings or additional interventions to optimize respiratory function and prevent further deterioration.
A respiratory rate of 22 breaths/min may be within an acceptable range, particularly considering that the patient is receiving mechanical ventilation. However, any significant deviation from the baseline respiratory rate or signs of respiratory distress, such as increased work of breathing or accessory muscle use, should be closely monitored and reported promptly.
B A heart rate of 106 beats/min may be within an acceptable range, although it is slightly elevated. Tachycardia can occur due to various factors, including pain, anxiety, fever, or hypoxemia. While tachycardia warrants close monitoring, it may not be the most critical finding to report unless it is associated with hemodynamic instability or other concerning symptoms.
C An oxygen saturation of 99% indicates adequate oxygenation, which is reassuring, particularly in a patient with acute respiratory distress syndrome (ARDS). However, oxygen saturation alone may not reflect the adequacy of ventilation or the severity of the underlying lung injury. Therefore, while oxygen saturation should be monitored closely, it may not be the most critical finding to report unless it declines significantly or is accompanied by other concerning symptoms.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
B This maneuver, called the Valsalva maneuver, can sometimes help to restore normal heart rhythm in cases of SVT. It involves blowing forcefully into a syringe or performing a similar action that increases intra-abdominal pressure, which can stimulate the vagus nerve and help to slow down the heart rate.
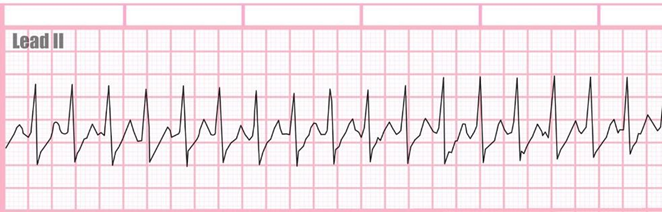
A Defibrillation is a treatment used for life-threatening cardiac arrhythmias, particularly ventricular fibrillation or pulseless ventricular tachycardia. It involves delivering a therapeutic dose of electrical energy to the heart with a device called a defibrillator.
C Drawing troponin levels may be appropriate if there is suspicion of myocardial infarction as the cause of chest palpitations or if there are other symptoms suggestive of acute coronary syndrome. However, in the context of SVT presenting with chest palpitations and a racing heart, the priority is to address the arrhythmia first
D Amiodarone is an antiarrhythmic medication used to treat various types of cardiac arrhythmias, including ventricular and supraventricular arrhythmias. While it can be effective in certain cases of SVT, it is not typically the first-line treatment or the immediate next step in managing SVT in the emergency department.
Correct Answer is B
Explanation
B. Assessing the client's vital signs, including blood pressure and pulse, provides critical information about the client's hemodynamic status and response to the new rhythm. Atrial fibrillation can lead to rapid, irregular heart rates and hemodynamic instability, so obtaining vital signs promptly helps the nurse determine the severity of the situation and whether immediate intervention is needed.
A. This action is not the priority when the nurse observes a new onset of atrial fibrillation. While beta- blockers such as metoprolol may be part of the client's long-term management for heart failure and atrial fibrillation, initiating medication administration without further assessment could delay appropriate intervention for the acute change in rhythm.
C. While it is important to communicate changes in the client's condition to the healthcare provider, this action should occur after the nurse has assessed the client's vital signs and determined the urgency of the situation. If the client is stable and responsive to initial interventions, the nurse can then contact the healthcare provider to discuss the new onset of atrial fibrillation and collaborate on further management.
D. Documenting the changes in the client's rhythm is important for continuity of care and communication among healthcare team members. However, obtaining a rhythm strip should not be the first action when a new onset of atrial fibrillation is observed. Assessing the client's vital signs and initiating appropriate interventions to address any hemodynamic instability take precedence.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
