A nurse is caring for a group of adolescents. Which of the following findings should be reported to the provider immediately?
A client who has a burn injury to an estimated 5% of his leg and is crying
A client who has an ankle fracture reports a pain level increase from 3 to 5 after initial ambulation
A who is a client 1 day postoperative and has a temperature of 37.5° C (99.5° F)
A client's blood pressure changes from 112/60 mm Hg to 90/54 mm Hg when standing
The Correct Answer is D
D. A client's blood pressure changes from 112/60 mm Hg to 90/54 mm Hg when standing.
A significant drop in blood pressure when changing positions from lying to standing may indicate orthostatic hypotension, which can be a sign of dehydration, blood loss, or other underlying medical issues. This can be a cause for concern, especially if the client is an adolescent, as it may lead to decreased perfusion of vital organs and may require immediate medical attention.
The other options are as follows:
A. A client who has a burn injury to an estimated 5% of his leg and is crying - While it's essential to assess and address the client's pain and comfort, this finding does not indicate an immediate need for medical attention. Pain management and wound care can be addressed based on the severity of the burn and the client's pain level.
B. A client who has an ankle fracture reports a pain level increase from 3 to 5 after initial ambulation - This finding is concerning, and the nurse should notify the provider to reassess pain management and evaluate for potential complications related to the fracture. However, it may not require immediate medical attention unless there are signs of severe pain or complications.
C. A client who is 1 day postoperative and has a temperature of 37.5° C (99.5° F) - A slight increase in temperature in the immediate postoperative period may not be unusual and can be attributed to the normal inflammatory response after surgery. The nurse should continue monitoring the client's temperature and report any further changes or additional signs of infection or complications to the provider.
Overall, while all findings should be addressed and managed appropriately, the significant drop in blood pressure (option D) should be reported immediately due to the potential implications for the client's overall health and well-being.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
For a 6-month-old infant who has undergone the repair of an intussusception, the nurse should select an oral electrolyte solution. This solution is specifically designed to replace lost fluids and electrolytes due to vomiting or diarrhea, which is crucial in preventing dehydration in infants.
Options A, B, and C are not suitable choices for an infant in this situation:
A. Half-strength orange juice: Citrus juices, including orange juice, are not recommended for infants under 12 months old. They are acidic and may cause stomach upset or diarrhea.
B. Sterile water: Sterile water does not contain the necessary electrolytes, and offering plain water to an infant after surgery or during an illness can lead to electrolyte imbalances and further dehydration.
C. Half-strength infant formula: Diluting infant formula can lead to inadequate nutrition for the infant. The baby requires appropriate nutrition to support recovery after surgery, and diluting formula can be harmful.
D. An oral electrolyte solution is the best choice as it helps maintain proper hydration and electrolyte balance in the infant's body during the recovery period. If the infant tolerates the oral electrolyte solution well and is not at risk for aspiration, the healthcare provider may gradually advance the diet to include other clear liquids and then slowly reintroduce regular infant formula or breast milk as appropriate. The healthcare provider's instructions should be followed carefully to support the infant's recovery and ensure adequate nutrition.
Correct Answer is B
Explanation
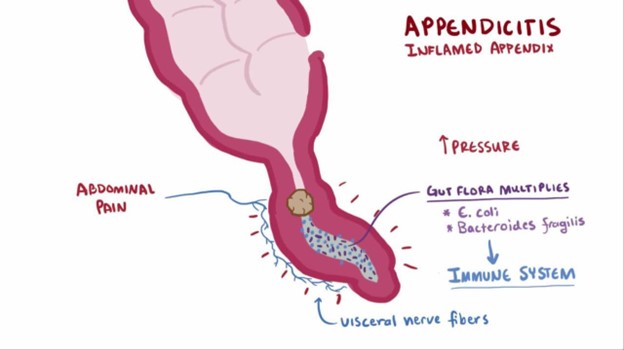
The nurse should clarify the prescription to administer sodium biphosphate/sodium phosphate because it is a laxative and is contraindicated in a child with suspected appendicitis. The use of laxatives or enemas can potentially worsen the condition by increasing the risk of perforation or rupture of the inflamed appendix.
A. Monitoring oral temperature every 4 hours is important to assess for signs of infection or worsening condition.
C. Maintaining NPO status is essential to avoid stimulating the digestive system and to prepare for possible surgery.
D. Medicating the client for pain every 4 hours as needed is appropriate to manage pain and provide comfort while the child awaits further evaluation or treatment.
Remember, it's crucial to avoid the use of laxatives, enemas, or any other interventions that can potentially aggravate the inflamed appendix in a child with suspected appendicitis.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
