A nurse is caring for an infant who has a congenital heart defect. Which of the following defects is associated with increased pulmonary blood flow?
Coarctation of the aorta
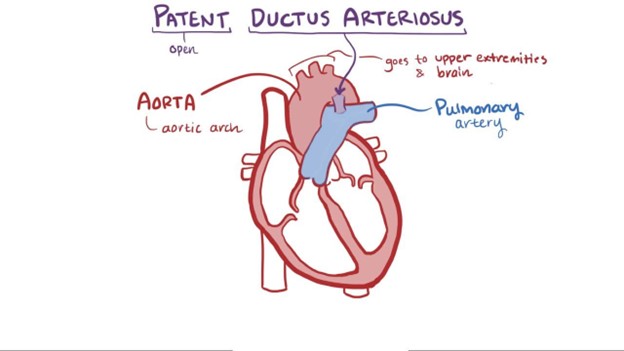
Patent ductus arteriosus
Tetralogy of Fallot
Tricuspid atresia
The Correct Answer is B
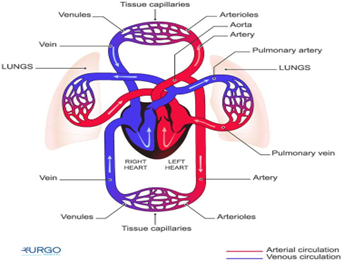
A patent ductus arteriosus (PDA) is a congenital heart defect associated with increased pulmonary blood flow. In normal fetal circulation, the ductus arteriosus allows blood to bypass the lungs since the baby receives oxygen from the mother's placenta. After birth, the ductus arteriosus should close, redirecting blood flow to the lungs for oxygenation. However, in some infants with PDA, the ductus arteriosus remains open, causing an abnormal connection between the aorta and the pulmonary artery. As a result, oxygenated blood from the aorta flows back into the pulmonary artery, increasing the workload on the lungs.
The other options are as follows:
A. Coarctation of the aorta - Coarctation of the aorta is a narrowing of the aorta, which obstructs blood flow and leads to increased blood pressure in the upper body and reduced blood flow to the lower body.
C. Tetralogy of Fallot - Tetralogy of Fallot is a combination of four heart defects that results in decreased pulmonary blood flow due to a ventricular septal defect (VSD), overriding aorta, pulmonary stenosis, and right ventricular hypertrophy.
D. Tricuspid atresia - Tricuspid atresia is a congenital heart defect where the tricuspid valve does not develop correctly, resulting in an absent or abnormal tricuspid valve. This defect prevents blood flow from the right atrium to the right ventricle and, therefore, reduces pulmonary blood flow.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
A. Gastrointestinal:
Kawasaki disease primarily affects blood vessels, and the gastrointestinal system is not the main target of this condition. While gastrointestinal symptoms can occur as part of the overall inflammatory response, such as abdominal pain, vomiting, or diarrhea, they are not the primary focus of concern in Kawasaki disease. The most critical system to monitor in Kawasaki disease is the cardiovascular system, specifically the coronary arteries.
B. Respiratory:
The respiratory system is not the primary system affected by Kawasaki disease. While respiratory symptoms can occur as part of the overall inflammatory response and fever associated with the disease, such as coughing or runny nose, they are not the main concern in Kawasaki disease. The primary system to monitor in this condition is the cardiovascular system, especially the coronary arteries.
C. Cardiovascular:
This is the correct answer. Kawasaki disease is primarily a vasculitis (inflammation of blood vessels) that affects various blood vessels, including the coronary arteries. The inflammation of the coronary arteries can lead to coronary artery aneurysms and other cardiac complications. Monitoring the cardiovascular system is essential to detect any signs of coronary artery involvement and ensure timely intervention to prevent potential long-term cardiac problems.
D. Integumentary:
The integumentary system (skin) is not the primary focus of Kawasaki disease. While some skin changes can occur during the acute phase of the disease, such as a rash or peeling skin on the hands and feet, these are not the primary concerns. Monitoring the cardiovascular system is critical in Kawasaki disease due to the risk of coronary artery inflammation and potential complications.
Correct Answer is A
Explanation
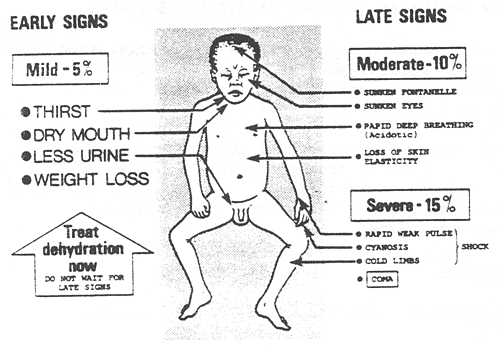
The nurse should expect to find irritability in an infant who is dehydrated. Dehydration in infants can lead to changes in behavior and irritability due to the imbalance in fluid and electrolytes. Other common signs of dehydration in infants may include:
Poor skin turgor (skin tenting)
Sunken fontanelles (soft spots on the baby's head)
Dry mucous membranes (dry mouth and tongue)
Decreased urine output or concentrated urine
Rapid heart rate (tachycardia)
Increased respiratory rate
Sunken eyes
Decreased tears when crying
B. Tetany is a condition characterized by involuntary muscle contractions and is more commonly associated with hypocalcemia (low calcium levels) rather than dehydration.
C. A slow, bounding pulse is not typically associated with dehydration. Dehydration often leads to a rapid heart rate (tachycardia) as the body attempts to compensate for the loss of fluid.
D. Decreased temperature is not a typical finding in dehydration. Dehydration can lead to fever in some cases due to an underlying infection, but it does not cause a decrease in body temperature on its own.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
