A nurse is caring for a client who has sustained a traumatic brain injury. The nurse should monitor the client for which of the following manifestations of increased intracranial pressure?
Tachypnea
Hypotension
Decreased level of consciousness
Bilateral weakness of extremities
The Correct Answer is C
Choice A: Tachypnea Tachypnea, or rapid breathing, is not typically a direct sign of increased ICP. While it can be associated with various medical conditions, it is not specifically indicative of increased ICP. However, it’s important to note that breathing patterns can change with advanced ICP changes, but these are usually characterized by irregularities rather than just increased rate. Increased intracranial pressure (ICP) is a critical condition that can occur after a traumatic brain injury (TBI). It results from the brain tissue’s response to injury, leading to swelling or bleeding within the skull. The skull is a rigid structure, so any increase in content, such as blood or edema, can lead to an increase in pressure.
Choice B: Hypotension Hypotension, or low blood pressure, is generally not associated with increased ICP. In fact, one of the signs of increased ICP is Cushing’s triad, which includes hypertension (high blood pressure), bradycardia (slow heart rate), and irregular respirations. Therefore, hypotension would not be a typical manifestation of increased ICP.
Choice C: Decreased level of consciousness A decreased level of consciousness is a hallmark sign of increased ICP. As pressure within the skull increases, it can lead to compression of the brain tissue and disruption of cerebral blood flow. This can manifest as changes in alertness, drowsiness, confusion, and in severe cases, loss of consciousness1. when monitoring a client who has sustained a TBI, the nurse should be vigilant for signs of increased ICP, with a decreased level of consciousness being a primary indicator. Other signs may include headache, nausea, vomiting, and changes in pupil size or reactivity. It is crucial to identify and treat increased ICP promptly to prevent further brain injury and potential long-term consequences.
Choice D: Bilateral weakness of extremities While bilateral weakness can be a sign of neurological damage, it is not specific to increased ICP. Increased ICP is more likely to cause global effects on consciousness and brain function rather than isolated weakness in limbs unless there is focal brain injury causing raised ICP.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
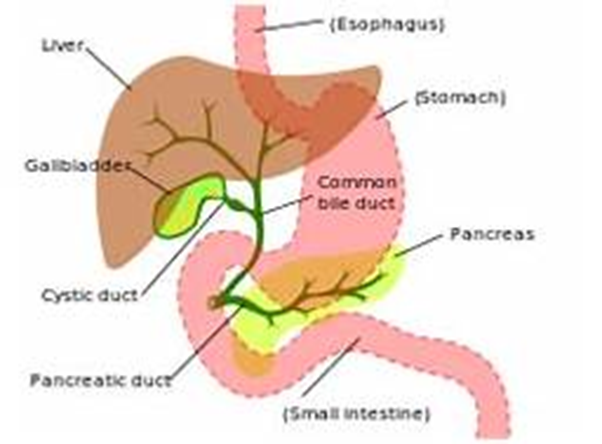
Choice A reason: Tenderness in the left upper abdomen is not typically associated with an obstruction of the common bile duct. This symptom is more commonly related to conditions affecting the stomach, pancreas, or spleen. The common bile duct is in the right upper quadrant of the abdomen, and tenderness in this area might be expected with its obstruction.
Choice B reason: Ecchymosis of the extremities is not a common finding in common bile duct obstruction. Ecchymosis, or bruising, is usually due to trauma, blood disorders, or other causes of fragile blood vessels and is not related to bile duct issues.
Choice C reason: Pale-colored urine is the opposite of what might be expected with common bile duct obstruction. Typically, the urine may become dark due to increased bilirubin levels that are excreted by the kidneys when the bile duct is obstructed.
Choice D reason: Fatty stools, or steatorrhea, are a classic finding in common bile duct obstruction. When bile flow is blocked, fats are not properly digested and absorbed, leading to stools that are bulky, greasy, and often have a foul odor. This occurs because bile is necessary for the emulsification and absorption of dietary fats in the intestine.
Correct Answer is B
Explanation
Choice A reason:Lower extremity edema is more commonly associated with right-sided heart failure, as it indicates systemic fluid congestion.
Choice B reason:Crackles in lung bases are expected in left-sided heart failure due to pulmonary congestion from fluid backing up into the lungs².
Choice C reason:Jugular vein distention is typically a sign of right-sided heart failure, reflecting increased central venous pressure.
Choice D reason:Ascites, the accumulation of fluid in the peritoneal cavity, is generally associated with right-sided heart failure or liver disease, not specifically left-sided heart failure.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
