A nurse is caring for a client who has quadriplegia from a spinal cord injury and reports having a severe headache. The nurse obtains a blood pressure reading of 210/108 mm Hg and suspects the client is experiencing autonomic dysreflexia. Which of the following actions should the nurse take first?
Administer a nitrate antihypertensive.
Obtain the client's heart rate.
Assess the client for bladder distention.
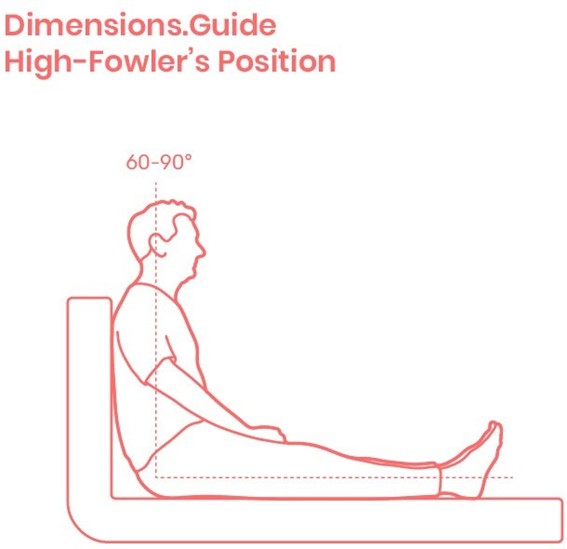
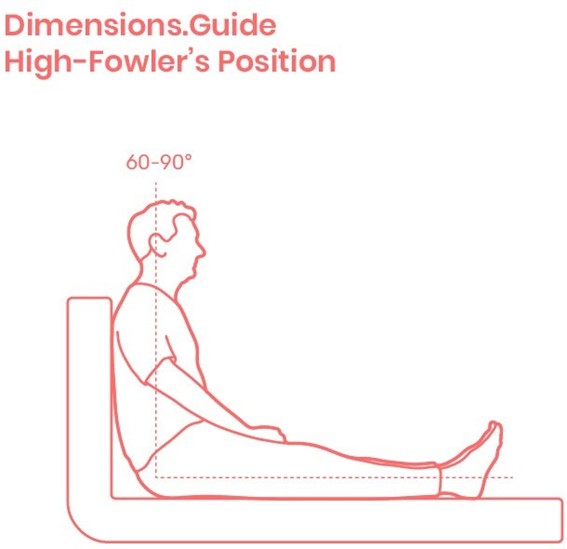
Place the client in a high-Fowler's position.
The Correct Answer is D
Choice A Reason: This is incorrect because administering a nitrate antihypertensive is not the first action, as it may cause a rapid drop in blood pressure and worsen the client's condition.
Choice B Reason: This is incorrect because obtaining the client's heart rate is not the first action, as it does not address the cause of autonomic dysreflexia or relieve the symptoms.
Choice C Reason: This is incorrect because assessing the client for bladder distention is not the first action, as it may take time and delay the treatment of autonomic dysreflexia.
Choice D Reason: This is correct because placing the client in a high-Fowler's position is the first action, as it lowers the blood pressure by promoting venous return and reducing cardiac preload.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A Reason: This is incorrect because administering a nitrate antihypertensive is not the first action, as it may cause a rapid drop in blood pressure and worsen the client's condition.
Choice B Reason: This is incorrect because obtaining the client's heart rate is not the first action, as it does not address the cause of autonomic dysreflexia or relieve the symptoms.
Choice C Reason: This is incorrect because assessing the client for bladder distention is not the first action, as it may take time and delay the treatment of autonomic dysreflexia.
Choice D Reason: This is correct because placing the client in a high-Fowler's position is the first action, as it lowers the blood pressure by promoting venous return and reducing cardiac preload.
Correct Answer is ["24"]
Explanation
- To find the concentration of heparin in the solution, divide the amount of heparin by the volume of D5W: 25,000 units / 500 mL = 50 units/mL
- To find the infusion rate, divide the prescribed dose by the concentration: 1,200 units/hr / 50 units/mL = 24 mL/hr
- Round the answer to the nearest tenth/whole number: 24 mL/hr
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
