A nurse is caring for a client on the medical-surgical unit. Laboratory Results. Vital Signs - Day 1 - 1200: Temperature 100.9°F (38.2°C), Respiratory Rate 26/min, Heart Rate 109/min, Blood Pressure 89/58 mmHg, Pain Score 9/10. Day 2 - Medication Administration - 0700: Temperature: 98.6°F (37°C), Heart Rate 98/min, Respiratory Rate 20/min, Record, Pain Score: 2/10, Blood Pressure 111/62 mmHg. Nurses' Notes - Vital Signs. Complete the diagram by dragging from the choices below to specify what condition the client is most likely experiencing. 2 actions the nurse should take to address that condition, and 2 parameters the nurse should monitor to assess the client's progress.
Hypocalcemia.
Hypernatremia.
Hyperkalemia.
Potential Condition. Action to Take 1: Prepare to check a serum albumin level. Action to Take 2: Request a STAT ECG. Parameters to Monitor 1: Serum bicarbonate level. Parameters to Monitor 2: Intake and Output.
The Correct Answer is A
Hypocalcemia. Action to Take 1: Prepare to check a serum albumin level.
Rationale:
Hypocalcemia can be influenced by changes in serum albumin levels, as calcium may bind to albumin. Correcting calcium levels based on albumin can help determine the actual calcium status. Action to Take 2: Request a STAT ECG. Rationale: Hypocalcemia can lead to prolonged QT intervals on an electrocardiogram (ECG). A STAT ECG is necessary to assess cardiac function and detect any potential arrhythmias. Parameters to Monitor 1: Serum bicarbonate level. Rationale: Monitoring serum bicarbonate levels can help assess the client's acid-base balance and metabolic status. Abnormal bicarbonate levels may indicate metabolic disturbances. Parameters to Monitor 2: Intake and Output. Rationale: Monitoring intake and output is essential to evaluate the client's fluid balance and kidney function. Hypocalcemia can impact renal function, and assessing urine output is crucial.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Cerebral bleeding. Choice A rationale:
Stress fractures are not directly related to hypernatremia. Hypernatremia is an electrolyte imbalance, and its main effects are related to cellular dehydration and neurological symptoms rather than bone fractures.
Choice B rationale:
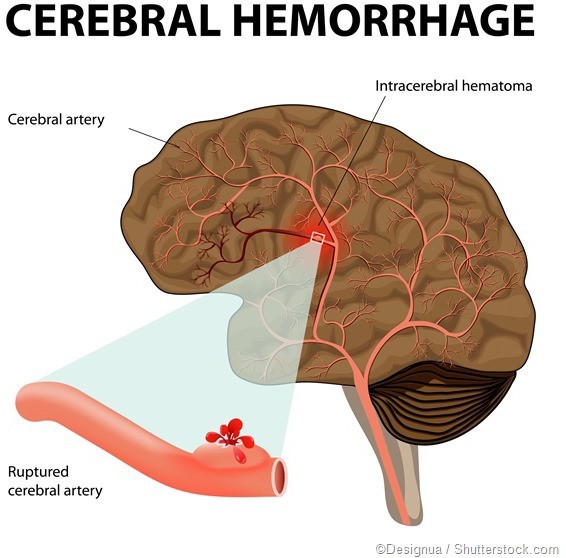
This is the correct answer because hypernatremia can lead to severe dehydration and cause neurological complications, including cerebral bleeding. The brain cells can shrink due to water loss, causing blood vessels to rupture, leading to bleeding in the brain.
Choice C rationale:
Atrial dysrhythmias are not directly associated with hypernatremia. Hypernatremia primarily affects the central nervous system and can lead to neurological symptoms rather than cardiac dysrhythmias.
Choice D rationale:
Pulmonary edema is not a likely consequence of hypernatremia. Pulmonary edema is associated with fluid volume excess, not fluid volume deficit, which is characteristic of hypernatremia.
Correct Answer is D
Explanation
Potential Condition.
Based on the provided information, it's challenging to make a definitive diagnosis with the given laboratory results and clinical presentation. The client's symptoms, such as severe abdominal pain, vomiting, dyspnea, yellow sclera, dry mucous membranes, tachycardia, and positive Chvostek and Trousseau signs, suggest a complex clinical picture that requires further investigation and assessment. Action to Take 1: Notify the provider. Rationale: The client's condition appears to be critical and requires immediate medical attention. Notifying the provider will initiate a comprehensive evaluation and potential interventions. Action to Take 2: Withhold medication for diarrhea until the underlying cause is determined. Rationale: Diarrhea can be a symptom of various conditions, and administering medication without a clear diagnosis may mask important clinical information. Parameters to Monitor 1: Serum bicarbonate level.
Rationale:
Monitoring serum bicarbonate levels can help identify potential acid-base imbalances and assess the client's metabolic status, especially given the history of end-stage renal disease. Parameters to Monitor 2: Intake and Output. Rationale: Monitoring intake and output is essential to assess fluid balance and kidney function, especially in a client with end- stage renal disease and potential electrolyte imbalances.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
