A nurse is assessing a full-term newborn upon admission to the nursery. Which of the following clinical findings should the nurse report to the provider?
Rust-stained urine.
Single palmar creases.
Subconjunctival hemorrhage.
Transient circumoral cyanosis
The Correct Answer is B
The correct answer is choice B. Single palmar creases.
Choice A rationale:
Rust-stained urine is typically due to urate crystals and is common in newborns. It usually resolves on its own and is not a cause for concern.
Choice B rationale:
Single palmar creases can be associated with certain genetic conditions, such as Down syndrome. This finding should be reported to the provider for further evaluation.
Choice C rationale:
Subconjunctival hemorrhage is a common finding in newborns due to the pressure changes during delivery. It usually resolves without intervention and is not typically a cause for concern.
Choice D rationale:
Transient circumoral cyanosis is often seen in newborns and can occur when the baby is crying or feeding. It usually resolves on its own and is not typically a cause for concern.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["3"]
Explanation
Use the following formula to calculate the amount of gentamicin to administer:
Volume (mL) = Dose (mg) / Concentration (mg/mL)
First, I need to convert the client's weight from pounds to kilograms. One pound is equal to 0.4536 kilograms. Therefore, 132 lb is equal to 132 x 0.4536 = 59.8752 kg.
Next, I need to multiply the client's weight by the prescribed dose of gentamicin per kilogram. The prescribed dose is 2 mg/kg, so the total dose is 2 x 59.8752 = 119.7504 mg.
Finally, I need to divide the total dose by the concentration of gentamicin in the injection. The concentration is 40 mg/mL, so the volume is 119.7504 / 40 = 2.99376 mL.
To round the answer to the nearest whole number, I need to look at the first decimal place. If it is 5 or more, I round up; if it is less than 5, I round down. In this case, the first decimal place is 9, which is more than 5, so I round up. Therefore, the final answer is 3 mL.
The nurse should administer 3 mL of gentamicin injection to the client.
Correct Answer is C
Explanation
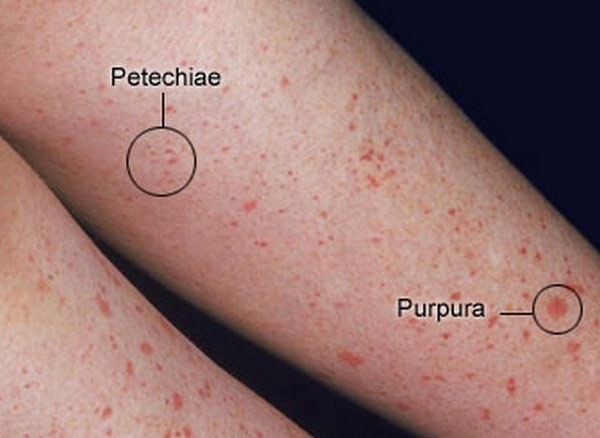
Facial petechiae are small, red or purple spots of bleeding under the skin or mucous membranes of the face. They are caused by the rupture of tiny blood vessels called capillaries. Facial petechiae can occur as a result of prolonged straining, such as during childbirth, vomiting, coughing, or crying¹. The increased pressure in the veins of the head and neck can cause the capillaries to burst, resulting in petechiae. Facial petechiae are usually harmless and resolve on their own without treatment.
The other options are not related to prolonged straining and have different causes and appearances:
a) Periauricular papillomas are benign, wart-like growths that occur near the ear. They are caused by human papillomavirus (HPV) infection and may be present at birth or develop later in life. They are usually painless and do not bleed⁴.
b) Erythema toxicum is a common skin condition in newborn babies. It causes a rash and small, fluid-filled bumps that may appear on the face, limbs, or chest. It is not caused by bleeding, infection, or allergy, but by an unknown mechanism. It does not cause discomfort to the baby and clears up without treatment within one to two weeks⁵.
d) Telangiectatic nevi are birthmarks that are caused by dilated blood vessels near the surface of the skin. They appear as red or purple patches or patterns on the skin that do not fade with pressure. They are present at birth and may grow in proportion to the child's growth. They are not associated with bleeding or infection and do not require treatment unless they cause cosmetic concerns⁶.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
