A nurse in a critical care unit is caring for a client who suffered a knife wound to the chest. The nurse suspects the client is developing cardiac tamponade. Which of the following assessment findings should the nurse identify as supporting this suspicion?
Flatened neck veins.
Bradycardia.
Sudden lethargy.
Muffled heart sounds.
The Correct Answer is D
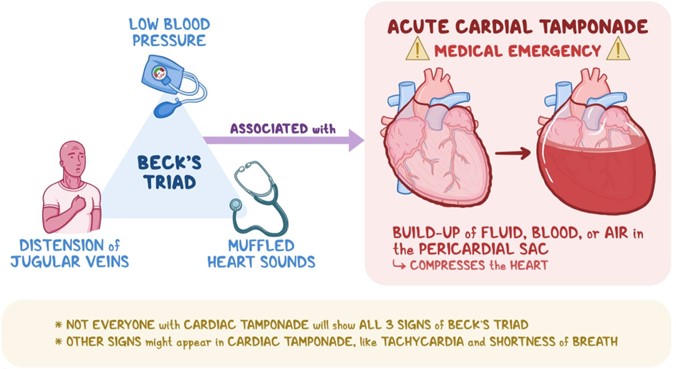
Choice A Reason: This choice is incorrect because flatened neck veins are not a sign of cardiac tamponade. Cardiac tamponade is a condition in which fluid accumulates in the pericardial sac that surrounds the heart, causing compression and impaired filling of the heart chambers. This leads to reduced cardiac output and hypotension. One of the manifestations of cardiac tamponade is distended neck veins due to increased venous pressure and impaired venous return.
Choice B Reason: This choice is incorrect because bradycardia is not a sign of cardiac tamponade. Bradycardia is a condition in which the heart rate is slower than normal (less than 60 beats per minute). It may be caused by various factors such as vagal stimulation, medication side effects, hypothyroidism, or sinus node dysfunction. It may cause symptoms such as fatigue, dizziness, or syncope, but it does not indicate cardiac tamponade.
Choice C Reason: This choice is incorrect because sudden lethargy is not a specific sign of cardiac tamponade. Lethargy is a condition in which the person feels tired, sluggish, or drowsy. It may be caused by various factors such as sleep deprivation, depression, infection, anemia, or hypoglycemia. It may affect the person's mental and physical performance, but it does not indicate cardiac tamponade.
Choice D Reason: This choice is correct because muffled heart sounds are a sign of cardiac tamponade. Muffled heart sounds are heart sounds that are fainter or softer than normal due to reduced transmission of sound waves through fluid-filled pericardial sac. They may indicate that the heart function is compromised by cardiac tamponade and require immediate intervention such as pericardiocentesis (removal of fluid from pericardial sac).
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["167 "]
Explanation
To calculate the dose of enoxaparin, follow these steps:
1) Convert the client's weight from pounds to kilograms:
245 lbs / 2.2046 (kg/lb) = 111.13 kg (rounded to the nearest whole number, it's 111 kg).
2) Multiply the weight in kilograms by the prescribed dose per kilogram:
111 kg x 1.5 mg/kg = 166.5 mg.
Round the answer to the nearest whole number, so the nurse should administer 167 mg per dose of enoxaparin every 12 hours to the client with a pulmonary embolism.
Correct Answer is B
Explanation
Choice A Reason: This choice is incorrect because hypomagnesemia is not a common finding in the oliguric phase of acute kidney injury. Hypomagnesemia is a condition in which the serum magnesium level is lower than normal (less than 1.5 mEq/L). It may be caused by various factors such as malnutrition, diarrhea, diuretics, or alcohol abuse. It may cause symptoms such as muscle weakness, tremors, tetany, or cardiac arrhythmias.
Choice B Reason: This choice is correct because hyperkalemia is a common finding in the oliguric phase of acute kidney injury. Hyperkalemia is a condition in which the serum potassium level is higher than normal (more than 5 mEq/L). It may be caused by reduced renal excretion of potassium due to decreased urine output (oliguria). It may cause symptoms such as muscle weakness, paresthesia, bradycardia, or cardiac arrest.
Choice C Reason: This choice is incorrect because decreased creatinine level is not a common finding in the oliguric phase of acute kidney injury. Creatinine is a waste product of muscle metabolism that is filtered by the kidneys and excreted in urine. A normal creatinine level ranges from 0.6 to 1.2 mg/dL for men and 0.5 to 1.1 mg/dL for women. In acute kidney injury, creatinine level usually increases due to reduced renal function and impaired clearance of creatinine.
Choice D Reason: This choice is incorrect because increased glomerular filtration rate (GFR) is not a common finding in the oliguric phase of acute kidney injury. GFR is a measure of how well
the kidneys filter blood and remove waste products.
A normal GFR range is 90,to 120 mL/min/1.73 m2. In acute kidney injury, GFR usually decreases due to reduced blood flow,to,the kidneys or damage to the glomeruli, which are the tiny blood vessels that filter blood in the kidneys.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
