A nurse in the emergency department is caring for a client who has extensive partial and full-thickness burns of the head, neck, and chest. While planning the client's care, the nurse should identify which of the following risks as the priority for assessment and intervention?
Infection
Airway obstruction
Paralytic ileus
Fluid imbalance
The Correct Answer is B
Choice A Reason: Infection is a serious complication of burn injuries, but not the priority risk for assessment and intervention. The nurse should monitor the client's wound healing, temperature, white blood cell count, and signs of sepsis, and administer antibiotics as prescribed. However, these measures are secondary to ensuring adequate oxygenation and ventilation.
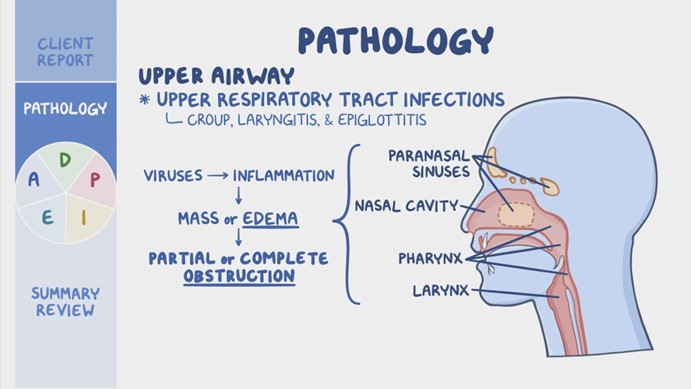
Choice B Reason: Airway obstruction is the priority risk for assessment and intervention for a client who has burns of the head, neck, and chest. The nurse should assess the client's airway patency, respiratory rate, oxygen saturation, breath sounds, and signs of respiratory distress, such as stridor, wheezes, or cyanosis. The nurse should also provide humidified oxygen, suction secretions, elevate the head of the bed, and prepare for endotracheal intubation if needed. Airway obstruction can occur due to edema, inflammation, or inhalation injury of the upper airway, and can quickly lead to hypoxia, respiratory failure, and death.
Choice C Reason: Paralytic ileus is a potential complication of burn injuries, but not the priority risk for assessment and intervention. The nurse should assess the client's bowel sounds, abdominal distension, nausea, vomiting, and stool output, and administer fluids, electrolytes, and nutritional support as prescribed. However, these measures are secondary to ensuring adequate oxygenation and ventilation.
Choice D Reason: Fluid imbalance is another potential complication of burn injuries, but not the priority risk for assessment and intervention. The nurse should assess the client's fluid status, urine output, vital signs, weight, and serum electrolytes, and administer intravenous fluids as prescribed. However, these measures are secondary to ensuring adequate oxygenation and ventilation.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A Reason: This choice is incorrect because inserting a central line is not a priority action for a client who has a sucking chest wound. A central line is a catheter that is inserted into a large vein in the neck, chest, or groin to administer fluids, medications, or blood products. It may be indicated for clients who have hypovolemia, sepsis, or shock, but it does not address the underlying cause of the client's respiratory distress.
Choice B Reason: This choice is incorrect because removing the dressing to inspect the wound may worsen the client's condition. A sucking chest wound is an open wound in the chest wall that allows air to enter and exit the pleural cavity with each breath. This creates a positive pressure in the pleural space that collapses the lung on the affected side and shifts the mediastinum to the opposite side, impairing the ventilation and circulation of both lungs. Therefore, the nurse should apply an occlusive dressing that covers three sides of the wound and allows air to escape but not enter the pleural cavity. Removing the dressing may allow more air to enter and increase the risk of tension pneumothorax, which is a life-threatening complication.
Choice C Reason: This choice is correct because administering oxygen via nasal cannula may help to improve the client's oxygenation and ventilation. A nasal cannula is a device that delivers oxygen through two prongs that fit into the nostrils. It can provide oxygen at low flow rates (1 to 6 L/min) and low concentrations (24 to 44 percent). The nurse should monitor the client's respiratory rate, pulse oximetry, and arterial blood gases to assess the effectiveness of oxygen therapy.
Choice D Reason: This choice is incorrect because raising the foot of the bed to a 90° angle may worsen the client's respiratory distress. This position may increase the pressure on the diaphragm and reduce the lung expansion. It may also decrease the venous return and cardiac output, leading to hypotension and shock. Therefore, the nurse should position the client in a semi-Fowler's position (30 to 45° angle) or high-Fowler's position (60 to 90° angle) to facilitate breathing and prevent further complications.

Correct Answer is D
Explanation
Choice A Reason: This is incorrect because magnesium 2.5 mEq/L is a normal value and does not indicate an increased risk of AKI. Magnesium is an electrolyte that plays a role in muscle and nerve function, blood pressure regulation, and energy production. The normal range for magnesium is 1.5 to 2.5 mEq/L.
Choice B Reason: This is incorrect because serum osmolality 290 mOsm/kg H2O is a normal value and does not indicate an increased risk of AKI. Serum osmolality is a measure of the concentration of solutes in the blood, such as sodium, glucose, and urea. The normal range for serum osmolality is 275 to 295 mOsm/kg H2O.
Choice C Reason: This is incorrect because blood urea nitrogen (BUN) 20 mg/dL is a normal value and does not indicate an increased risk of AKI. BUN is a measure of the amount of urea, a waste product of protein metabolism, in the blood. The normal range for BUN is 7 to 20 mg/dL.
Choice D Reason: This is correct because serum creatinine 1.8 mg/dL is an elevated value and indicates an increased risk of AKI. Creatinine is a waste product of muscle metabolism that is filtered by the kidneys. The normal range for serum creatinine is 0.6 to 1.2 mg/dL for women and 0.7 to 1.3 mg/dL for men. An increase in serum creatinine indicates a decrease in kidney function and glomerular filtration rate (GFR).
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
